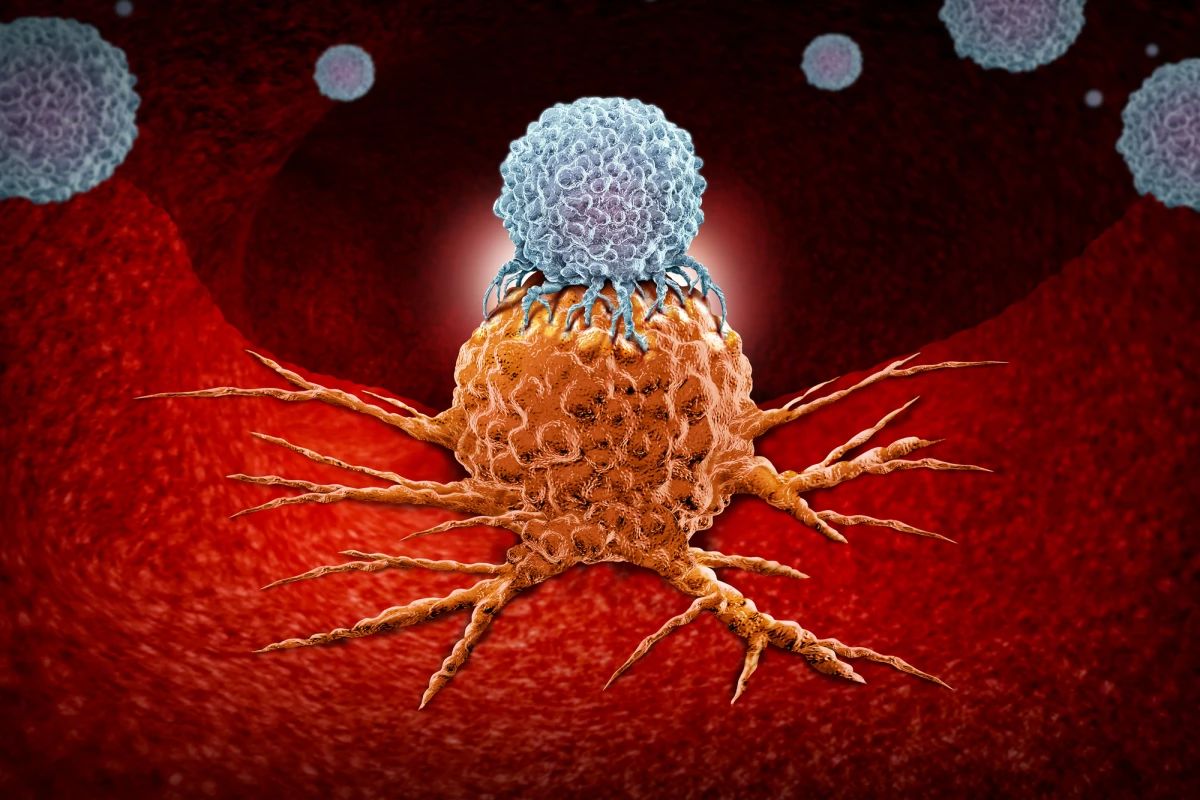
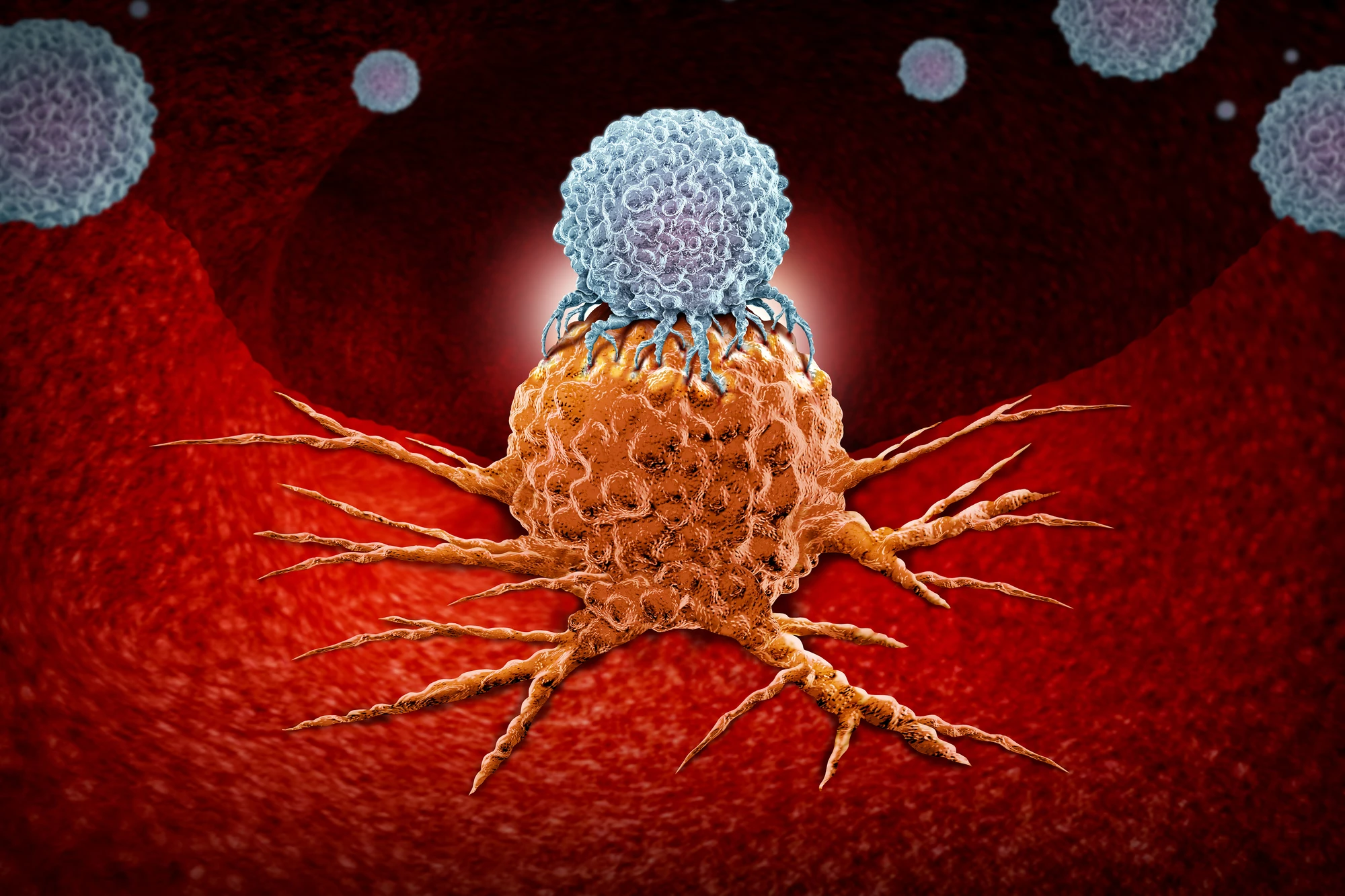
Constantly fighting cancer or other diseases can exhaust our immune system’s T cells, impeding their ability to kill invaders. A new study has identified a way of reviving exhausted T cells so they’re ready to fight again, improving the effectiveness of cancer immunotherapy.
A type of white blood cell, T cells play an important role in protecting the body from foreign invaders such as cancer. But they can only fight for so long before they become exhausted. When this happens, T cells don’t produce as many immune-response-stimulating proteins and are less effective at killing cancer tumor cells.
Immunotherapy is the umbrella term for a range of biologically based cancer treatments that uses T cells to fight cancer by boosting the immune system’s ability to stop or slow cancer cell growth or help it recognize and destroy cancer cells. For immunotherapy to be effective requires T cells to be in peak – non-exhausted – condition.
Researchers at Sanford Burnham Prebys in California studied T cell exhaustion in the setting of melanoma and discovered that a protein called P-selectin glycoprotein ligand-1 (PSGL-1), found on the surface of T cells, is key to T cell exhaustion.
“Slowing or reversing T cell exhaustion is a huge focus in cancer research, and many researchers are working on different ways to accomplish this,” said Jennifer Hope, lead author of the study. “This new approach could be a viable treatment on its own, but it also has tremendous potential to work synergistically with existing therapies.”
The approach is unique because it tackles the problem of T cell exhaustion from multiple angles.
After studying mice with a genetic deficiency in PSGL-1, the researchers found that the protein causes T cell exhaustion and that T cell exhaustion was slowed by an antibody that blocked PSGL-1 activity in mice with immunotherapy-resistant melanoma. They also noticed that exhausted T cells regained their function.
“One of the things that makes this approach unique compared to existing immunotherapies is that it directly alters the way T cells become exhausted and helps them regain their function,” Hope said.
After seeing success using their antibody-based approach on mice with melanoma, the researchers tested it on mice with mesothelioma, an aggressive and deadly form of cancer that usually affects the lung tissues and is linked to asbestos exposure. They found that their approach worked with that type of cancer, too.
The next step for the researchers is to adapt their approach so that it’s suitable for use in humans with the potential that it can be used to treat a wide range of treatment-resistant cancers.
“Once we’ve done all the necessary science, this could be really valuable, or even lifesaving, for a lot of people with cancers that are resistant to current treatments,” said Linda Bradley, corresponding author of the study. “We still have a long way to go, but I’m optimistic that we’re onto something game-changing here.”
The study was published in the journal Cell Reports.
Source: Sanford Burnham Prebys