A next-generation cancer vaccine has shown stunning results in mice, preventing up to 88% of aggressive and difficult-to-treat cancers by harnessing dual-pathway nanoparticles that train the immune system to recognize and destroy tumor cells.
Melanoma, pancreatic cancer, and triple-negative breast cancer (TNBC) are each serious clinical challenges due to how common or aggressive they are and how poorly they often respond to treatment. Which is why scientists are determined to develop an effective treatment for all of them.
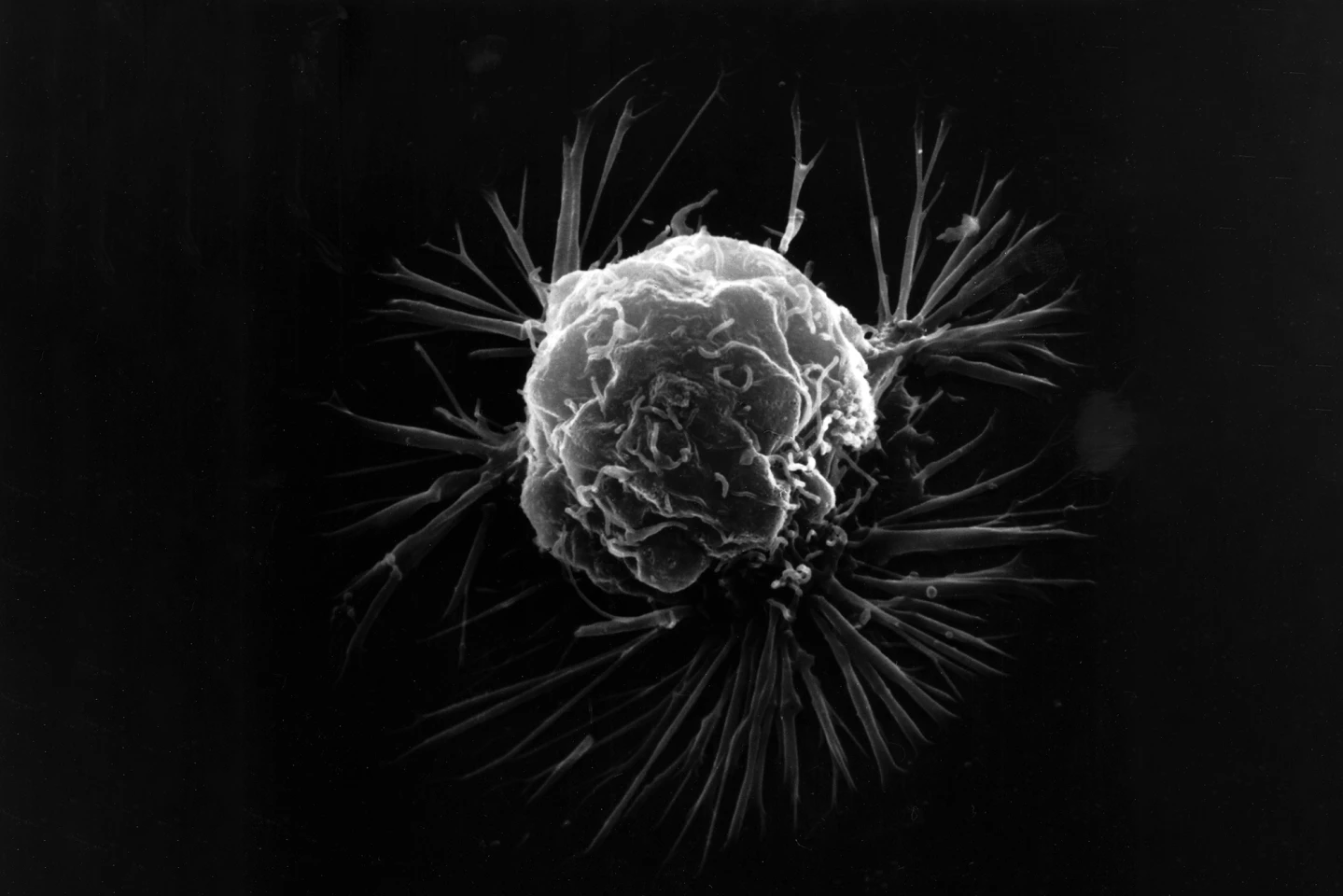
A new study led by University of Massachusetts (UMass) Amherst researchers has brought us a step closer to achieving this, with their immune-stimulating nanoparticle-based vaccine that effectively prevented melanoma, pancreatic cancer and TNBC in mice.
“By engineering these nanoparticles to activate the immune system via multi-pathway activation that combines with cancer-specific antigens, we can prevent tumor growth with remarkable survival rates,” said Prabhani Atukorale, PhD, assistant professor of biomedical engineering in the Riccio College of Engineering at UMass Amherst and the study’s corresponding author.
The vaccine combines two immune-stimulating molecules (adjuvants) in a tiny lipid nanoparticle that enhances both innate and adaptive immune responses. The innate immune system acts as the body’s first line of defense, responding quickly and non-specifically to invaders using cells that release inflammatory signals. The adaptive immune system takes longer to activate but provides a targeted, long-lasting response, training T cells and B cells to recognize and remember specific threats. Together, they form a coordinated defense: the innate system alerts and activates the adaptive system, which then delivers precise and durable immunity.
Mice were vaccinated subcutaneously (under the skin) using a prime-boost-boost schedule on days 0, 14, and 35. Vaccines were combined either with tumor peptides (specific antigens from melanoma) or with whole tumor cell lysates (a mix of tumor proteins, to mimic real tumors). The researchers then tested the vaccine in three aggressive cancer models: melanoma, pancreatic cancer, and TNBC. They also measured how well the nanoparticles reached lymph nodes, where immune responses are activated, and how well they activated key immune messengers called dendritic cells, and generated T-cell and B-cell responses.
The dual-adjuvant nanoparticles produced an enhanced, effective immune response in the mice. They also drained efficiently to the lymph nodes, which is essential for vaccine effectiveness, and activated dendritic cells. When combined with multiple peptides, 100% of vaccinated mice rejected tumors, while all untreated or single-adjuvant groups died within a month. Mice that survived the first tumor challenge remained tumor-free after being re-challenged months later, providing evidence of long-term immune memory.
“Metastases across the board is the highest hurdle for cancer,” Atukorale said. “The vast majority of tumor mortality is still due to metastases, and it almost trumps us working in difficult-to-reach cancers, such as melanoma and pancreatic cancer. That is a real advantage of immunotherapy, because memory is not only sustained locally. We have memory systemically, which is very important. The immune system spans the entire geography of the body.”
Using whole tumor lysate instead of defined peptides led to protection across melanoma, pancreatic, and breast cancer models. Between 69% and 88% of mice remained tumor-free after challenge, and all survived a second systemic tumor challenge. Both T cells and B cells contributed to the immune response, suggesting the vaccine provided broad, multi-arm immunity.
“The tumor-specific T-cell responses that we are able to generate – that is really the key behind the survival benefit,” said Griffin Kane, postdoctoral research associate at UMass Amherst and the lead author of the study. “There is really intense immune activation when you treat innate immune cells with this formulation, which triggers these cells to present antigens and prime tumor-killing T cells.”
The researchers envision their vaccine being used as both a treatment and a preventive, and as an approach to treating multiple cancer types. To help them in this endeavor, Atukorale and Kane created a startup called NanoVax Therapeutics.
“The real core technology that our company has been founded on is this nanoparticle and this treatment approach,” Kane said. “This is a platform that Prabhani developed. The startup lets us pursue these translational efforts with the ultimate goal of improving patients’ lives.”
The study was published in the journal Cell Reports Medicine.
Source: UMass Amherst






