A compelling new study from scientists at McGill University has, for the first time, described precise microbiome alterations that can be confidently correlated with fibromyalgia, a disease fundamentally characterized by widespread chronic pain.
Fibromyalgia was only officially defined as a medical condition in 1990, and it is still a relatively mysterious disorder with no clear diagnostic test. It is generally classified as a disorder of the central nervous system, characterized by heightened sensitivity to pain and excessive pain across a number of different parts of the body.
The new research was inspired by the rapidly expanding body of evidence uncovering correlations between the gut and the brain. A team from McGill University hypothesized there may be a relationship between the composition of the gut microbiome and those suffering from this relatively inexplicable disease.
A cohort of 77 women with fibromyalgia were recruited, against a control of 79 healthy subjects. Microbiome samples were extensively analyzed and the results revealed those fibromyalgia subjects displayed clearly identifiable microbiome compositions, distinct from those in the healthy control group.
"We used a range of techniques, including artificial intelligence, to confirm that the changes we saw in the microbiomes of fibromyalgia patients were not caused by factors such as diet, medication, physical activity, age, and so on, which are known to affect the microbiome," explains first author on the study, Amir Minerbi.
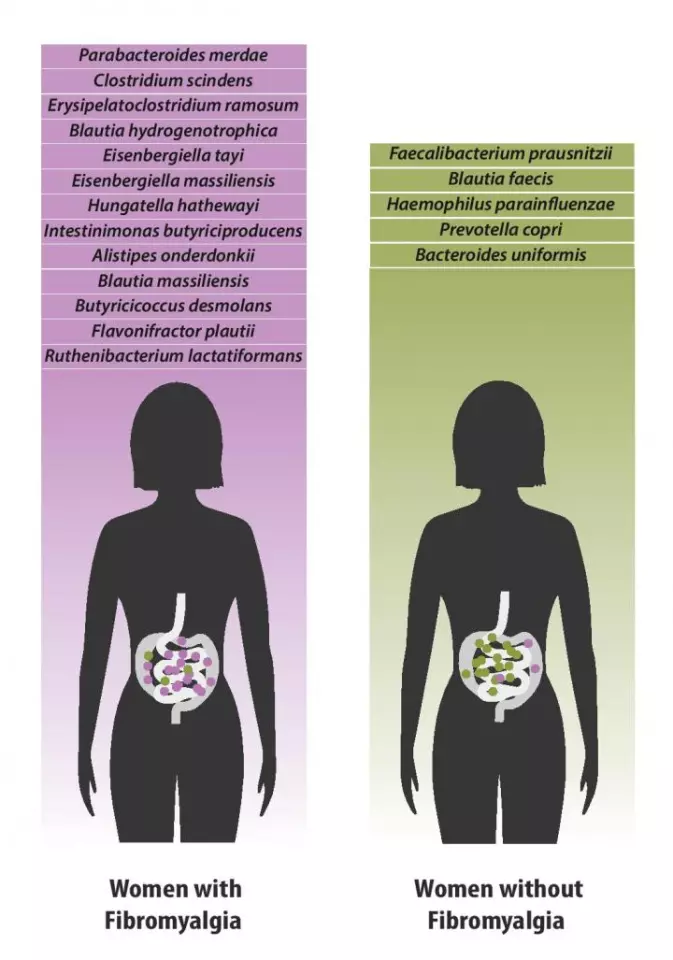
The study revealed 19 differentially abundant specific species of gut bacteria in the fibromyalgia subjects. Faecalibacterium prausnitzii, for example, was one species noted in lower abundance. This bacterial species has also interestingly been found to be depleted in patients with chronic fatigue syndrome. Bacteroides uniformis, another depleted species, has previously been implicated in inflammatory arthritis.
The specific microbiome blueprint for fibromyalgia described in the study was unique when compared to microbiome compositions described in other conditions such as inflammatory bowel disease, and even more specifically, the researchers were able to correlate the severity of the condition with the presence, or absence, of certain bacteria. This led the scientists to use this microbiome blueprint to generate a diagnostic process that could incredibly accurately identify fibromyalgia patients just from their gut bacteria.
"By using machine learning, our computer was able to make a diagnosis of fibromyalgia, based only on the composition of the microbiome, with an accuracy of 87 per cent," says Emmanuel Gonzalez, a researcher on the project. "As we build on this first discovery with more research, we hope to improve upon this accuracy, potentially creating a step-change in diagnosis."

The researchers are very clear in noting the study does not suggest these gut bacterial markers play a causal role in the onset of pain related to fibromyalgia and a great deal more work is necessary to uncover any potential causal mechanism at play. What this novel study does offer, however, is a useful road map directing future research pathways. As fibromyalgia is primarily a disease related to chronic non-visceral pain, it will be fascinating to watch scientists explore how directly some of these bacterial species associate with other expressions of chronic pain, such as neuropathy or lower back pain.
Looking at more immediate outcomes from this research, the machine-learning classification system developed in the study suggests an incredibly useful potential new way to diagnose a condition that currently has no standard, objective diagnostic criteria.
The new research was published in the journal Pain.
Source: McGill University





