In a recent experiment that sounds more sci-fi than science class, researchers have successfully developed a novel vaccine platform that uses ordinary dental floss embedded with tiny dissolvable microneedles. The study, published in Nature Biomedical Engineering, showcases how everyday materials can be reimagined to offer adaptable and accessible vaccine solutions.
Researchers at North Carolina State University and the University of North Carolina at Chapel Hill have developed a microneedle-thread platform designed to deliver vaccine antigens through oral mucosal tissue. In preclinical trials, they investigated whether this approach could induce both local and systemic immune responses – a strategy intended to enhance protection against pathogens that enter through the respiratory tract.
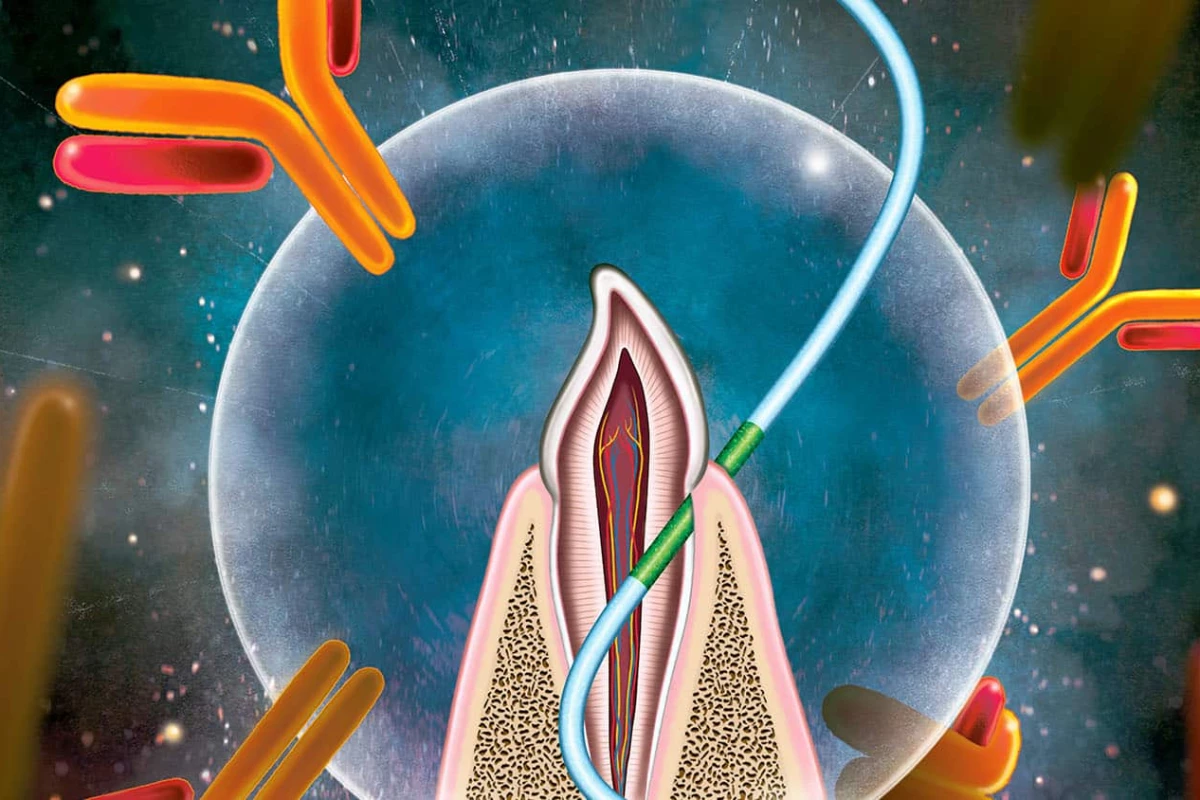
This new method targets the junctional epithelium, the “leaky” tissue where gums meet teeth. On any given day, this permeable region serves as an immunological checkpoint, allowing immune cells to surveil for bacteria accumulating along the gumline. Intrigued by its natural permeability, researchers asked a deceptively simple question: could this oral gateway be repurposed to deliver vaccines?
To put their idea to the test, the team turned to the lab, where they conducted controlled experiments in mice to assess delivery through the gingival sulcus – a permeable, densely vascularized tissue with direct access to immune surveillance. Instead of syringes, they used a strand of floss: biodegradable threads embedded with dissolvable microneedles designed to deliver antigens directly into the tissue (imagine that on your resume: mouse flosser intern).
The results were striking. Mice that received vaccines via floss developed strong immune responses across multiple arms of immunity: mucosal antibodies, systemic antibodies, and T cells. These responses were achieved using a variety of vaccine formats, including protein antigens, inactivated virus, nanoparticles, and mRNA. In one trial, all mice vaccinated against influenza using the floss-based method survived a normally lethal viral challenge, while the unvaccinated mice did not.
What makes this unconventional vaccination site so effective comes down to its biology. Unlike skin, which acts as a tight physical barrier, the junctional epithelium is naturally porous.
“This is a unique gateway,” explained Harvinder Singh Gill, corresponding author of the study and professor of nanomedicine at North Carolina State University. “Mucosal surfaces are a common entry point for respiratory pathogens like influenza and COVID. Delivering a vaccine here allows us to generate immune responses not only in the bloodstream, but also right where the pathogen tries to enter.”
This dual-action response is pivotal. Traditional injected vaccines typically stimulate systemic immunity alone. But when delivered at mucosal sites, vaccines can also produce local antibodies, such as IgA, which coat mucosal membranes in the nose, throat, and lungs; creating a first line of defense.
To explore whether this method could translate to humans, the researchers conducted a pilot study using floss picks impregnated with dye in place of the vaccine. Volunteers then used the floss picks to work the dye into their gums at the gingival sulcus. In about 60% of participants, the dye was successfully deposited – a promising sign that human tissue may be similarly receptive to this oral delivery route.
That said, the technique wouldn’t apply to infants and toddlers who lack teeth, and researchers note that its performance in people with gum disease or oral infections remains an open question.
If further research confirms safety and efficacy in humans, floss-based vaccines might one day serve as a supplemental tool, targeting respiratory viruses at their point of entry. While further testing is needed, the study serves as a reminder that medical innovation doesn’t always require high-tech solutions, sometimes it just takes repurposing a common tool.
This study was published in the journal Nature: Biomedical Engineering.