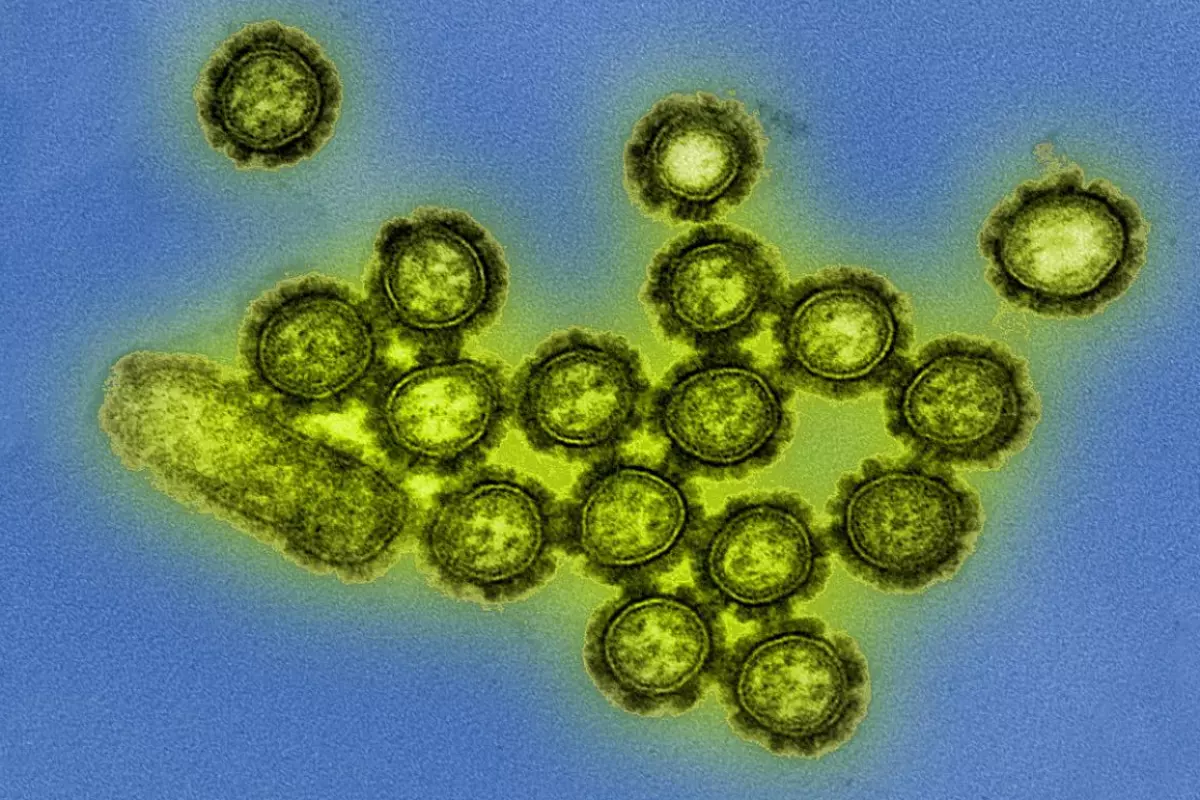
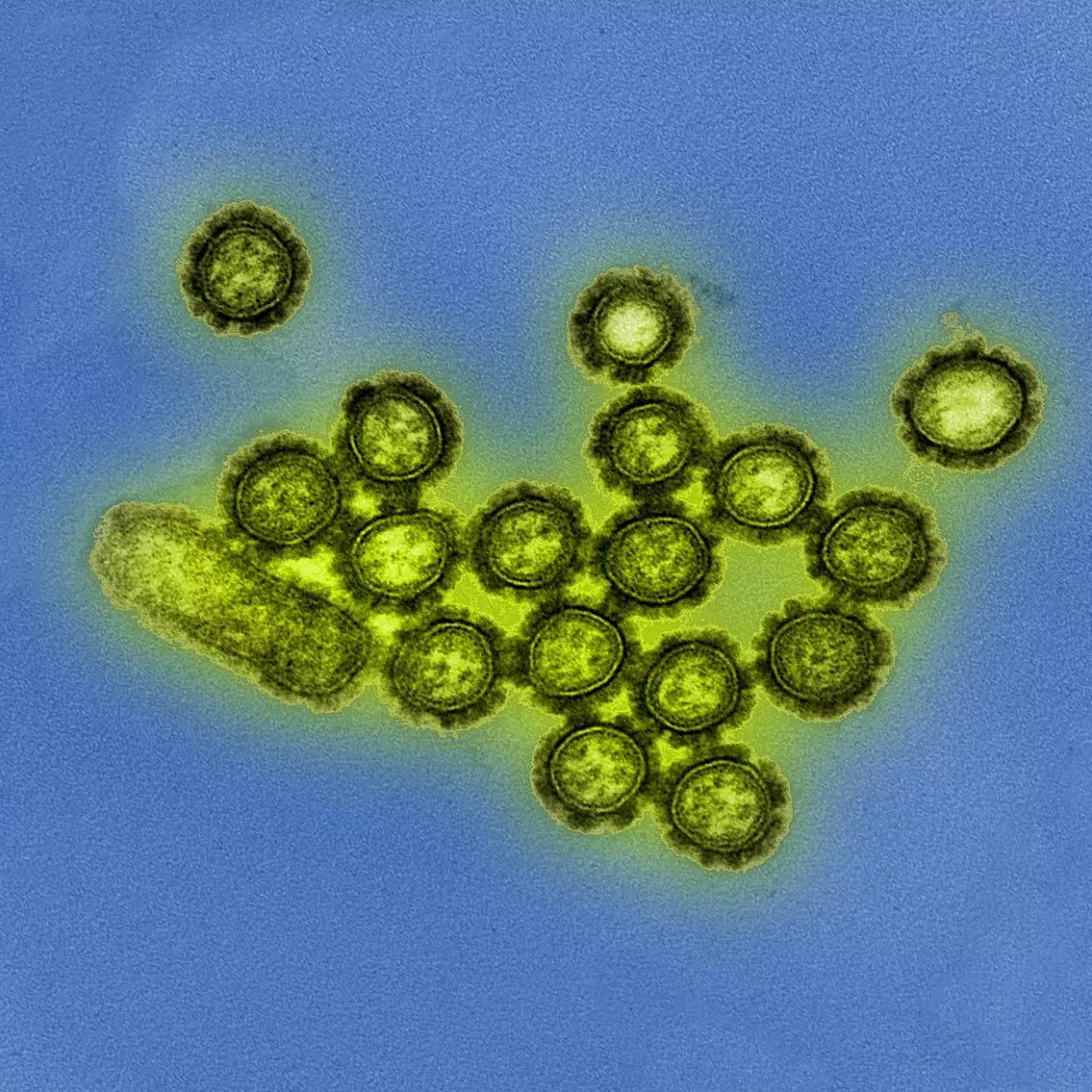
A new study is offering the first evidence in humans to suggest depletion of gut microbiome diversity by antibiotics can reduce the efficacy of a vaccination. The research focused on a cohort administered with the influenza vaccine, hypothesizing gut bacteria to play a central role in immune response to vaccinations.
Last year a team of Australian researchers presented a mouse study finding antibiotics can severely impair an animal’s immune response to vaccinations. That research focused on young mice as proxies for human babies in their first year of life, and specifically examined five vaccines given routinely to infants, including meningitis and whooping cough.
An earlier Stanford study from 2011 found similar impaired immune responses in animal studies, particularly when mice were bred with no gut microbiome. Despite these studies associating microbiome with vaccine efficacy, until now no human studies had been conducted to examine the phenomenon.
“To our knowledge, this is the first demonstration of the effects of broad-spectrum antibiotics on the immune response in human – in this case, our response to vaccination – directly induced through the disturbance of our gut bacteria,” says Bali Pulendran, who worked on the 2011 Stanford research, and is senior author on the newly published study.
The new research first investigated a cohort of 22 adults during the 2014-15 flu season. Half the subjects received the flu vaccine as normal, while the other half were administered a trio of broad-spectrum antibiotics for five days immediately before getting the vaccine.
Unsurprisingly, the antibiotic group showed a 10,000 fold reduction in gut bacteria diversity, but more interestingly, both groups showed comparable levels of influenza-preventing antibodies 30 days after vaccination. The researchers discovered both cohorts displayed high-levels of targeted protective influenza antibodies before vaccination. This suggested the subjects may have previously been exposed to the specific strains of flu in the 2014-15 vaccine.
Those making up the second cohort investigated in the study the following year were specifically selected to make sure they indicated low-levels of antibodies to the specific strains in that year’s vaccine. The experiment was repeated, but this time the antibiotic group showed significantly lower antibody responses to one particular strain in the flu vaccine.
What this result suggested to the researchers is the subjects may have had no prior exposure to this particular flu strain. So while it seems antibiotics don't influence your immune memory to previously confronted pathogens, it does affect one’s ability to generate immunity to a new pathogen.
“The study indicates that when it comes to responding to vaccination against a previously encountered infectious pathogen, our immune systems are remarkably resilient even in the face of the most severe depletion of our intestinal bacteria,” says Pulendran. “But they seem to lose this resilience when confronted with a vaccine containing new pathogenic elements of which they have little or no prior memory.”
In some ways this research is good news for those worried about whether antibiotics can directly reduce immune responses to illnesses from old vaccinations. The study does suggest immune memory can hold strong in the face of short-term microbiome disruptions. However, the study also implies fresh vaccine-induced immune responses can certainly be impaired in the face of acute microbiome disruptions from antibiotics. Pulendran doesn’t explicitly suggest we avoid taking antibiotics in close proximity to vaccinations. More research certainly needs to be done to better understand the mechanisms that may be at play, but he does remind people to get a flu shot regardless of antibiotic status.
“Get your annual flu shot,” say Pulendran. “The greater your inventory of immune memory to influenza strains bearing any resemblance to the one that’s coming over the hill, the more likely you’ll be able to deal with it, even if your gut microbes are in short supply.”
The new study was published in the journal Cell.
Source: Stanford Medicine