Studying the effects of drugs and disease in humans can be tricky business, but scientists are making great inroads in developing lab-grown versions of organs and body parts that offer powerful platforms for experimentation. Research in this area has now led to first-of-a-kind bone marrow “organoids” that bear the key features of the real thing and that their creators hope can lead to a new breed of bespoke treatments for cancer.
By using stem cells as a starting point, scientists have managed to produce lab-grown versions of an impressive array of human body parts. The list so far includes brains, blood vessels and lungs, and is growing rapidly, with these miniaturized models serving as next-gen research tools to study disease and develop drugs that can improve outcomes for patients.
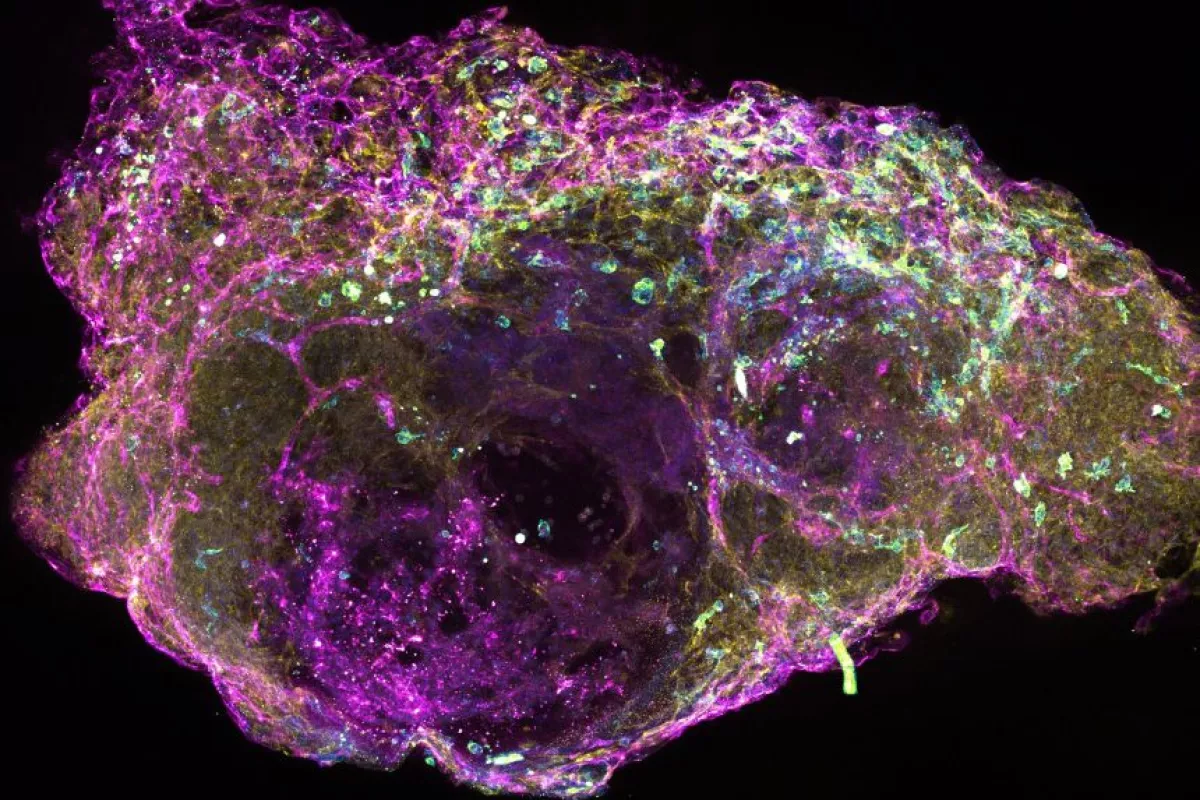
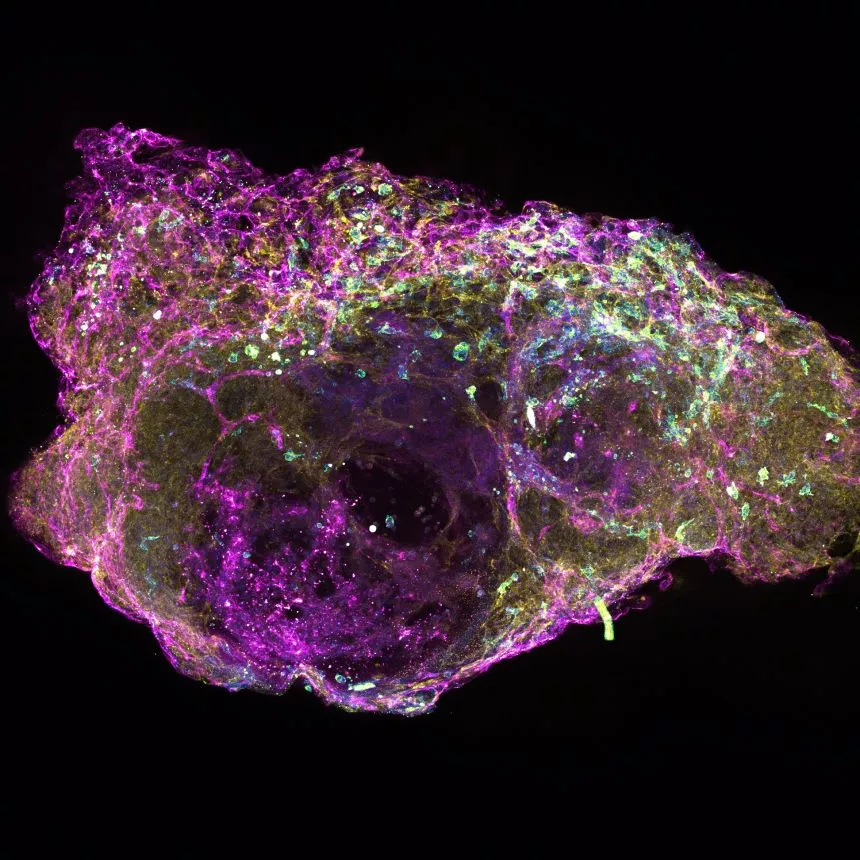
Scientists at Oxford University and the University of Birmingham are now claiming another first in this area. The team took human stem cells and grew them in a purpose-built 3D scaffold designed to drive their maturation into the key cell types you’d find in living human bone marrow.
“Remarkably, we found that the cells in their bone marrow organoids resemble real bone marrow cells not just in terms of their activity and function, but also in their architectural relationships – the cell types ‘self-organize’ and arrange themselves within the organoids just like they do in human bone marrow in the body,” said first author of the study Dr Abdullah Khan.
These are described as the first bone marrow organoids to include all the key components of human bone marrow, and because bone marrow serves as the production house for circulating blood cells, the organoids are already providing valuable insights. For example, the scientists were able to use organoids to study how the cells in bone marrow facilitate the generation of these blood cells. Further, they were able to study how the process is hampered by bone marrow fibrosis, or the buildup of scar tissue.
“Developing a protocol that enabled us to grow the organoids reproducibly and at scale was a challenge, particularly as we were working between labs in Birmingham and Oxford over the pandemic, so I spent a lot of time frantically driving organoids down the A40,” said Khan. “However, we are thrilled with the results, as we now have a platform that we can use to test drugs on a personalized medicine basis.”
The organoids could offer important new insights into the development of blood cancer. The scientists were able to use them to keep cancer cells from blood cancer patients alive in the lab, which has historically been a challenge. This raises the prospect of developing customized treatments that are designed for specific patients, using their own cancer cells as a starting point.
“To properly understand how and why blood cancers develop, we need to use experimental systems that closely resemble how real human bone marrow works, which we haven’t really had before,” said senior study author Professor Bethan Psaila. “It’s really exciting to now have this terrific system, as finally, we are able to study cancer directly using cells from our patients, rather than relying on animal models or other simpler systems that do not properly show us how the cancer is developing in the bone marrow in actual patients.”
The research was published in the journal Cancer Discovery.
Source: University of Oxford