Researchers have used molecular imaging technology to confirm maternal vitamin D levels' crucial role in developing the brain cells that produce dopamine, the body’s ‘feel-good’ chemical. The finding provides a greater understanding of the mechanisms underlying neurodevelopmental disorders like schizophrenia.
Schizophrenia is thought to develop as a result of a combination of genetic and environmental factors. The precise mechanism by which it does so is unknown, but there is strong evidence to suggest that the condition causes a change in how the brain uses dopamine.
It’s thought that exposure to risk factors for schizophrenia during embryonic development alters how dopamine circuits are formed in the brain. Previous studies have found that low levels of maternal vitamin D are one such risk factor, affecting how dopamine-producing (dopaminergic) neurons differentiate into their mature, specialized form.
A team of researchers at the University of Queensland’s Brain Institute have built on past research to more closely investigate the link between vitamin D, dopaminergic neurons, and schizophrenia with the help of molecular imaging technology.
The scientists created dopamine-like neurons to replicate the differentiation process that occurs during an embryo’s development. The neurons were cultured with and without the hormone calcitriol. Ingested vitamin D is inactive until it undergoes two enzymatic reactions in the body, the second of which occurs in the kidney, where it is converted into calcitriol, the active form of vitamin D. Calcitriol binds to and activates the vitamin D receptor in the cell’s nucleus.
The researchers discovered that vitamin D not only affected cell differentiation, but it also affected the neuron’s structure.
“What we found was the altered differentiation process in the presence of vitamin D not only makes the cells grow differently but recruits machinery to release dopamine differently,” said Darryl Eyles, corresponding author of the study.
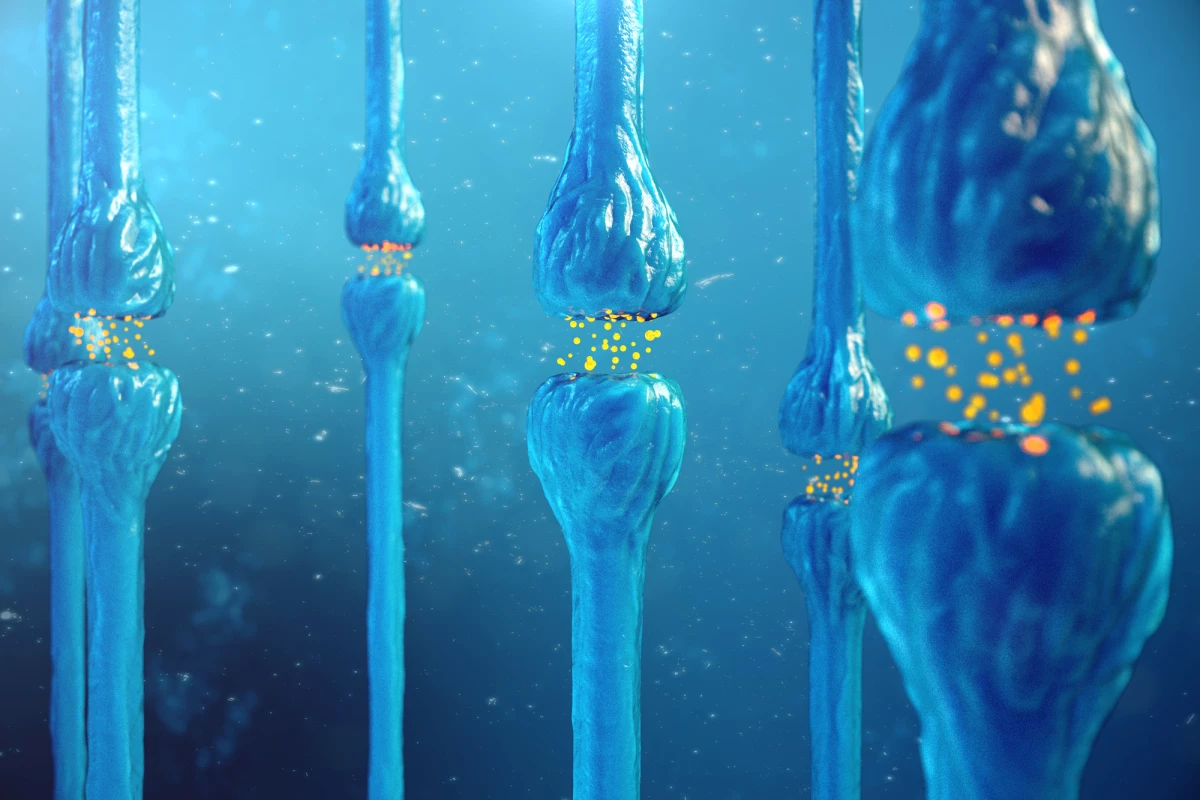
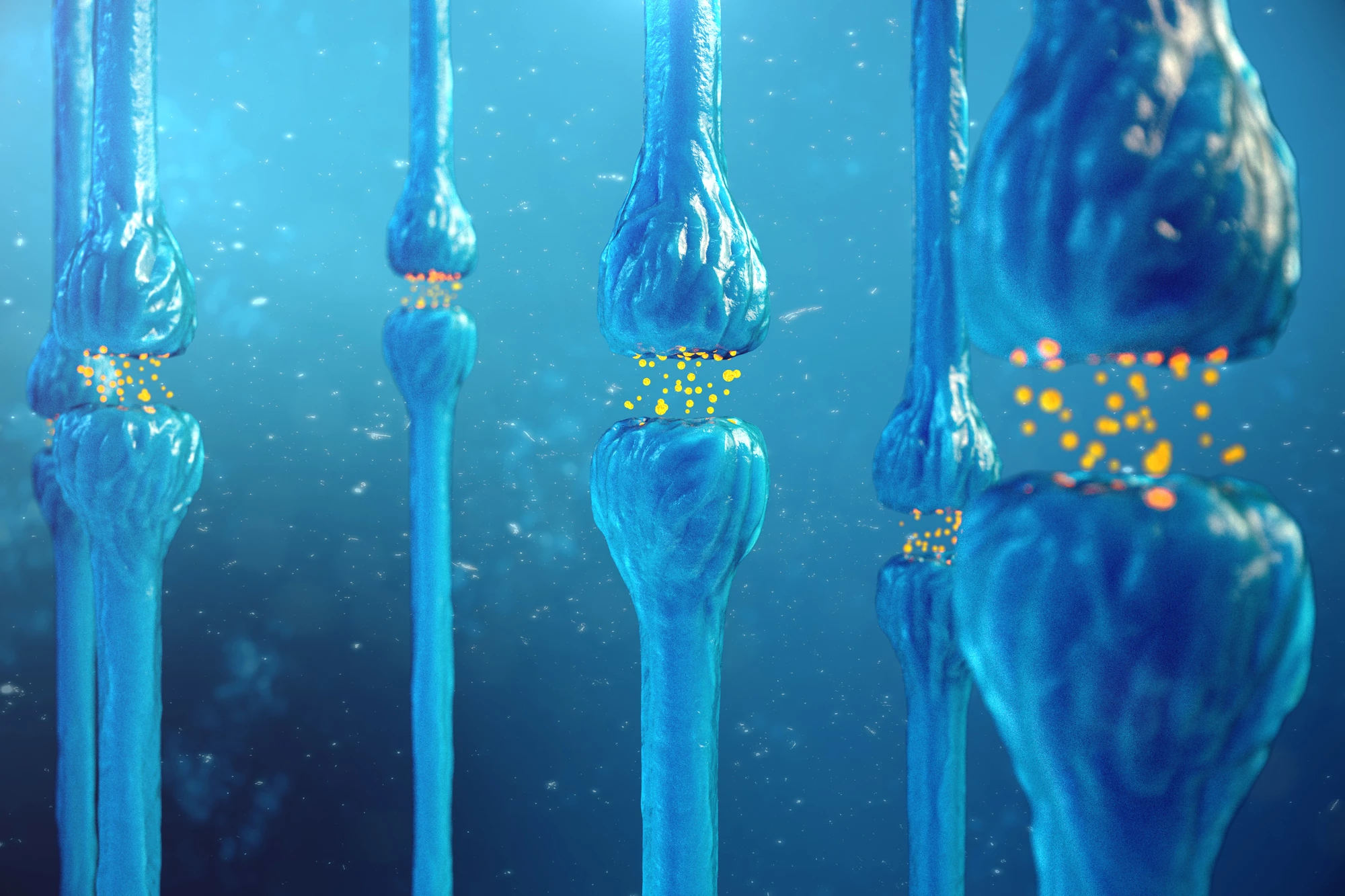
The "machinery" are neurites, projections that grow out from the cell body of a neuron. Neurites are required to send and receive signals to and from other parts of the nervous system. The researchers found that the number of neurites was markedly increased, and within those neurites, the distribution of the proteins responsible for releasing dopamine was altered.
Using a new imaging tool called false fluorescent neurotransmitters (FFNs), the researchers could analyze how dopamine uptake and release changed in the presence or absence of calcitriol. FFNs are small-molecule dyes that closely imitate the action of a neurotransmitter, such as dopamine. They enable the imaging of both the storage and release of single molecules at nerve terminals.
They found that, compared to a control, dopamine release was enhanced in neurons grown in the presence of calcitriol.
“This is conclusive evidence that vitamin D affects the structural differentiation of dopaminergic neurons,” Eyles said.
Using FFNs to target and observe single dopamine molecules has meant that the researchers could confirm their long-standing belief that vitamin D levels during development affect how dopamine-producing neurons are formed. They believe early changes in dopamine neuron differentiation and function may lead to the dopamine dysfunction seen in adult schizophrenia.
The researchers plan to investigate whether other environmental risk factors for schizophrenia, such as low oxygen levels or infection during pregnancy, also alter how dopamine neurons develop.
The study was published in the Journal of Neurochemistry.
Source: University of Queensland