In a fascinating discovery, scientists have pinpointed what happens in our brains when we're expecting pain relief but are given a placebo, unknowingly, instead. It not only confirms 'the placebo effect,' but offers clues into how powerful the mind is in mitigating physiological functions such as pain.
Pain research has long been hampered by experiment design, in which even trials that are double-blinded and randomized will still see those who receive placebo treatment reporting some relief from their unknown medication. But until now, scientists haven't really known just what is happening in the brain when this occurs.
In a study led by researchers from the University of North Carolina (UNC) School of Medicine, along with Stanford, the Howard Hughes Medical Institute and the Allen Institute for Brain Science, a pathway that travels from the cortex to the cerebellum reveals just how an individual may feel pain relief without any analgesic intervention.
“That neurons in our cerebral cortex communicate with the pons and cerebellum to adjust pain thresholds based on our expectations is both completely unexpected, given our previous understanding of the pain circuitry, and incredibly exciting,” said Greg Scherrer, from the UNC School of Medicine. “Our results do open the possibility of activating this pathway through other therapeutic means, such as drugs or neurostimulation methods to treat pain.”
The researchers first identified, through imaging, regions of the brain that had a boost of activity, but it wasn't clear exactly what was happening – just that something was definitely happening. From here, they undertook an intricate study on mice to home in on the mechanisms at play.
In that mouse study, the researchers found that along the pathway, from the front of the brain, through the pons region of the brainstem to the cerebellum at the rear, neurons and synapses became very active when pain-relief was anticipated, regardless of whether any real medicine was then taken.
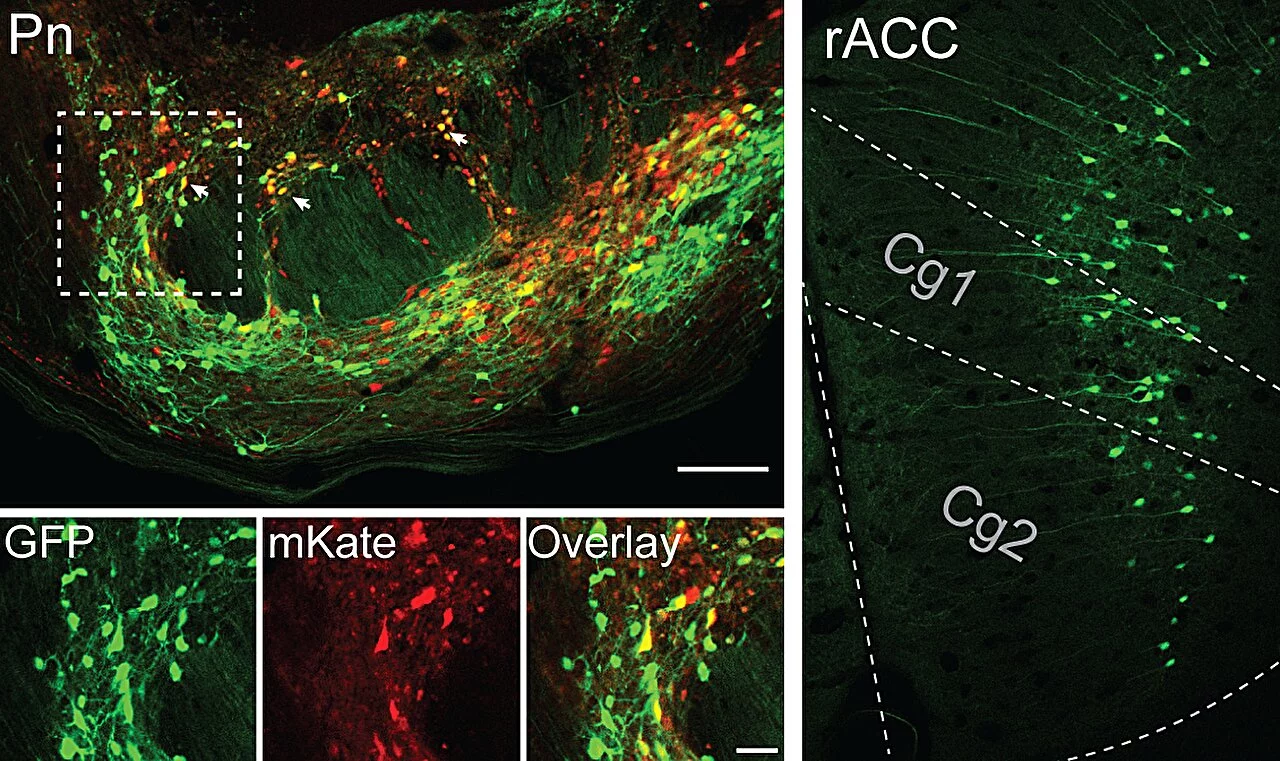
Looking at the anterior cingulate cortex (ACC), which has been linked to the placebo effect in pain studies, the scientists used a suite of methods to unravel the mystery: genetically tagged neurons, imaging to view calcium in neurons, single-cell RNA sequencing techniques, electrophysiological recordings and optogenetics.
What they found was that when mice received an innocuous dose of medicine, instead of pain relief, the rostral ACC neurons signaled to the pontine nucleus – which has no prior link to pain or pain relief – and along the pathway other signals had been activated.
“There is an extraordinary abundance of opioid receptors here, supporting a role in pain modulation,” Scherrer said. “When we inhibited activity in this pathway, we realized we were disrupting placebo analgesia and decreasing pain thresholds. And then, in the absence of placebo conditioning, when we activated this pathway, we caused pain relief."
They found that the large, branch-like Purkinje cells in the cerebellum replicated the activity seen in the initial area of neuronal excitement, in the ACC. It confirmed that the cerebellum had a key part to play in pain messaging.
The findings do more than just solve a puzzle for neuroscientists and put to bed any thought that the placebo effect was 'all in your head' (even though, quite literally, it is). The researchers believe it has the potential for new approaches to pain relief, including chronic disorders, which have proven challenging to treat effectively.
“We all know we need better ways to treat chronic pain, particularly treatments without harmful side effects and addictive properties,” Scherrer said. “We think our findings open the door to targeting this novel neural pain pathway to treat people in a different but potentially more effective way.”
The study was published in the journal Nature.






