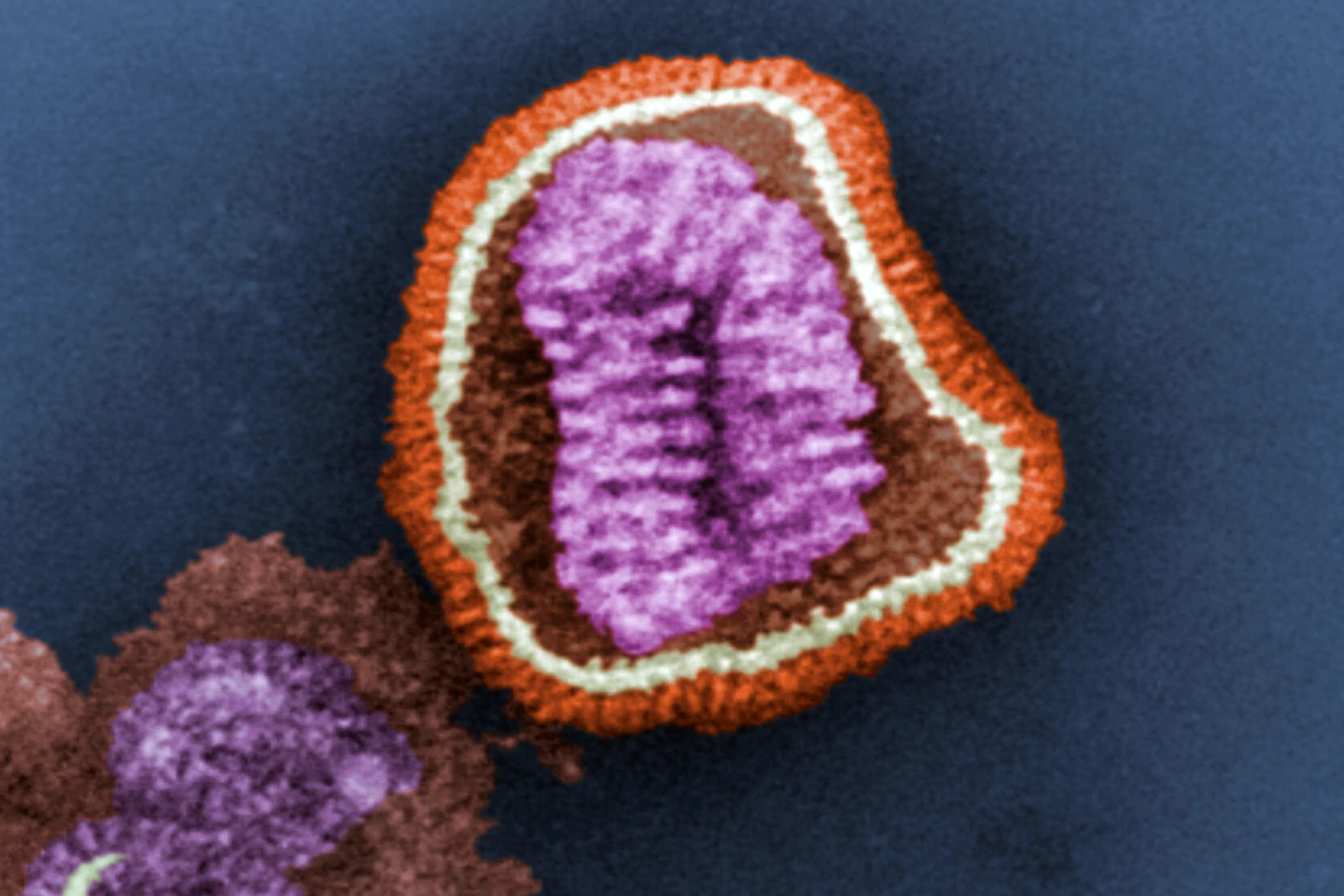
If you’ve ever caught the flu, you’ve more than likely been infected with the Influenza A virus (IAV). Compared to the Influenza B virus, infection with the A type often produces more severe symptoms. But, while many of us have experienced the fever and chills, headache and muscle aches, fatigue, sore throat and cough of a run-of-the-mill flu, severe infection with IAV is a different, potentially life-threatening beast.
Severe IAV infection triggers a specific type of cell death, necroptosis, in infected cells. While it’s a natural process designed to limit viral spread by actively eliminating infected cells and mobilizing the immune system to respond, necroptosis can activate a hyper-inflammatory response, causing collateral lung damage that’s potentially lethal. Other than managing its symptoms, few therapeutic options are available to treat severe flu.
In a new study, researchers from Tufts University School of Medicine, St Jude’s Children’s Research Hospital, University of Houston, and Fox Chase Cancer Center worked together to test a drug named UH15-38 that prevented this flu-related lung injury in mice while still allowing the immune system to fight the virus.
“Our drug significantly increased survival and lowered symptoms of influenza virus infection,” said Paul Thomas, co-corresponding author and St Jude’s Host-Microbe Interactions faculty member. “It dampened dangerous inflammation and even seemed to improve the adaptive response against the virus.”
Achieving the drug’s ‘Goldilocks effect’ on inflammation required the researchers to employ some clever chemistry combined with a thorough understanding of the mechanisms underpinning necroptosis.
Receptor interacting protein kinase 3 (RIPK3) is an essential part of the necroptotic cell death pathway but also controls another cell death pathway: apoptosis. Both types of cell death produce opposing immune responses. Apoptotic death usually leads to immunologically silent responses, whereas necroptosis releases molecules that promote inflammation. UH15-38 was designed to prevent RIPK3 from triggering the necroptotic pathway – and, therefore, runaway inflammation – while still allowing apoptotic cell death, removing infected cells in a less inflammatory way.
“If you remove necroptosis, you still get restriction of the viral replication without causing the massive damage to the lungs,” said Alexei Degterev, associate professor of developmental, molecular and chemical biology at Tufts University School of Medicine and co-corresponding author of the study. “Necroptosis does not appear to be necessary for restricting a viral activity, so if we can block it, we will be able to protect the host by reducing inflammation in the lungs.”
The researchers tested UH15-38 on mouse models and found that a high dose of the drug protected against a dose of IAV that would ordinarily be fatal. And, at low doses, UH15-38 protected the mice from similar amounts of influenza that humans experience. Notably, the mice were protected even if they received the drug days after infection with IAV.
“This drug can … do something we’ve never seen before,” Thomas said. “We’re able to start five days after the initial infection and show that we’re still providing some benefit. Knocking out RIPK3 entirely is not great because then the immune system can’t clear the virus. When we knocked out just necroptosis, the animals did better because they still had apoptosis and could still get rid of infected cells, but it wasn’t as inflammatory.”
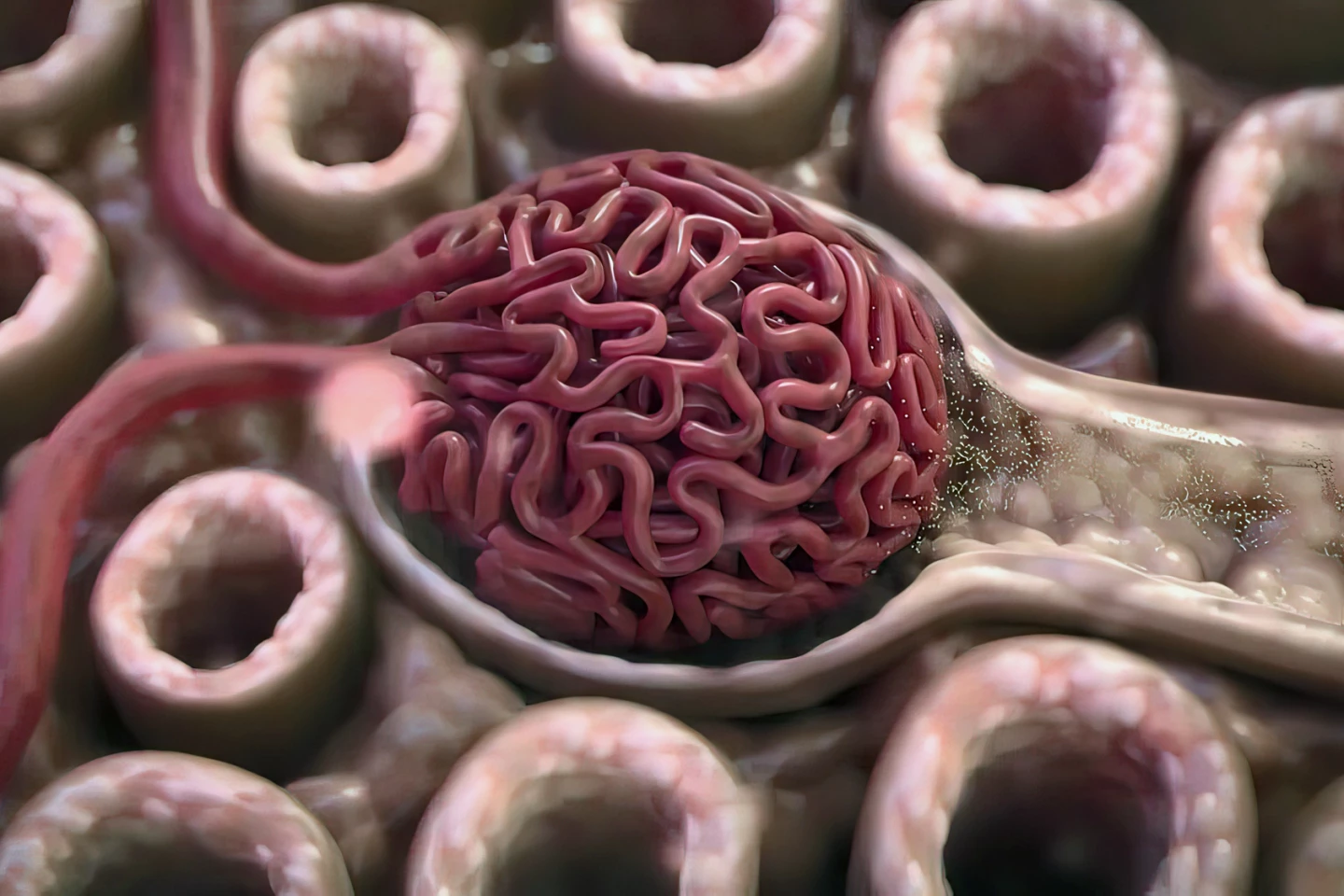
UH15-38 improved survivability by preventing necroptosis’ collateral damage to type 1 alveolar epithelial cells, a specific cell type in the lungs that facilitates gas exchange. Damage to these cells can make it difficult to get oxygen into the blood and carbon dioxide out of it, producing symptoms such as shortness of breath, wheezing and chest tightness. The drug also reduced the number of inflammation-related immune cells, such as neutrophils, in the mice.
“Often, the worst part of influenza illness happens after the virus is controlled when runaway inflammation destroys lung cells,” said Thomas. “UH15-38 can dampen that influenza-caused inflammation while leaving viral clearance and the other functions of the immune and tissue responses intact. That makes it a promising candidate to move forward toward the clinic.”
Safely tolerated by the mice, the next step is further preclinical and human trials of UH15-38. The researchers are testing whether UH15-38 is effective in treating other respiratory diseases while working on the second generation of RIPK3 inhibitors. Tufts University’s Office for Tech Transfer and Industry Collaboration is managing the commercialization of UH15-38.
“While the worst of COVID-19 may be behind us, the credible expectation is that there will be another pandemic that’s going to happen, and we need something that is going to protect the host independent of how the host is infected,” said Degterev. “This work highlights the possibility of achieving such a goal and renews interest in how cell death shapes infections.”
The study was published in the journal Nature.
Sources: Tufts University School of Medicine, St Jude’s Children’s Research Hospital via EurekAlert!







