Preliminary research, from scientists at Case Western Reserve University, has discovered several blood-based biomarkers which can specifically indicate stroke damage to brain tissue. The goal of the research is to develop a simple blood test to rapidly detect whether a patient is suffering a minor stroke.
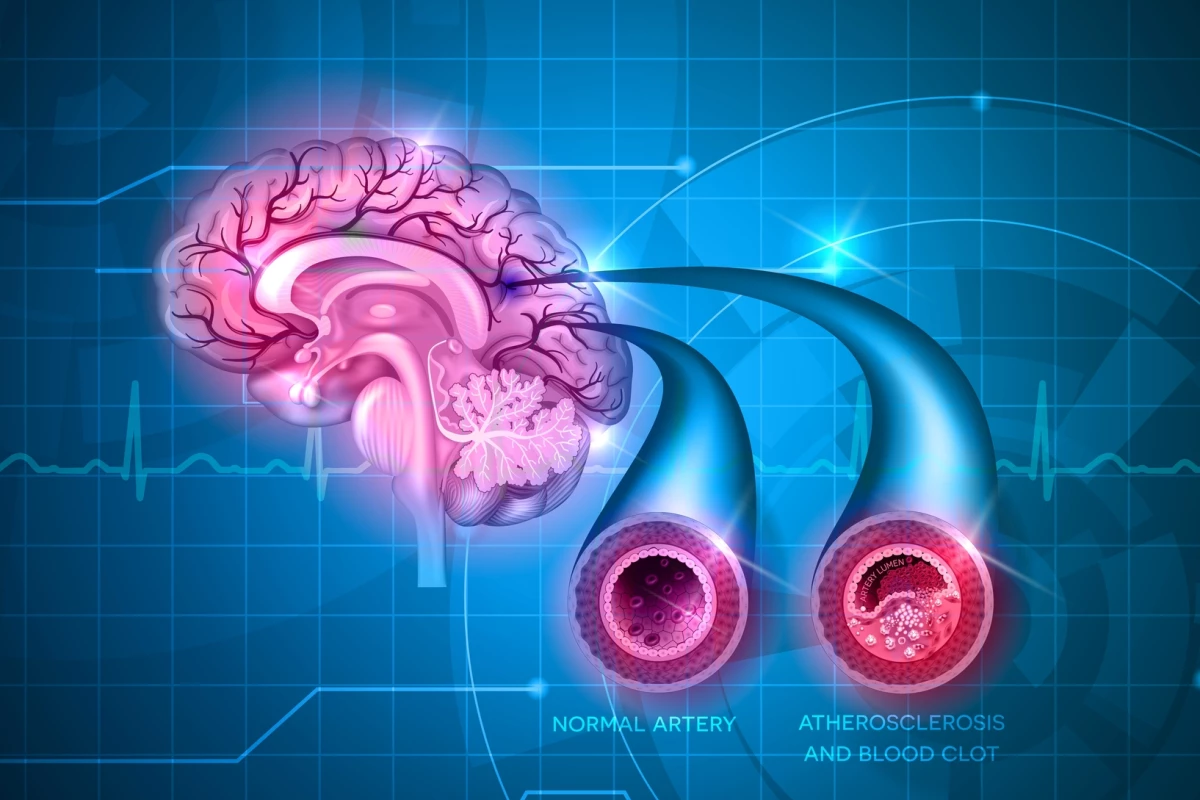
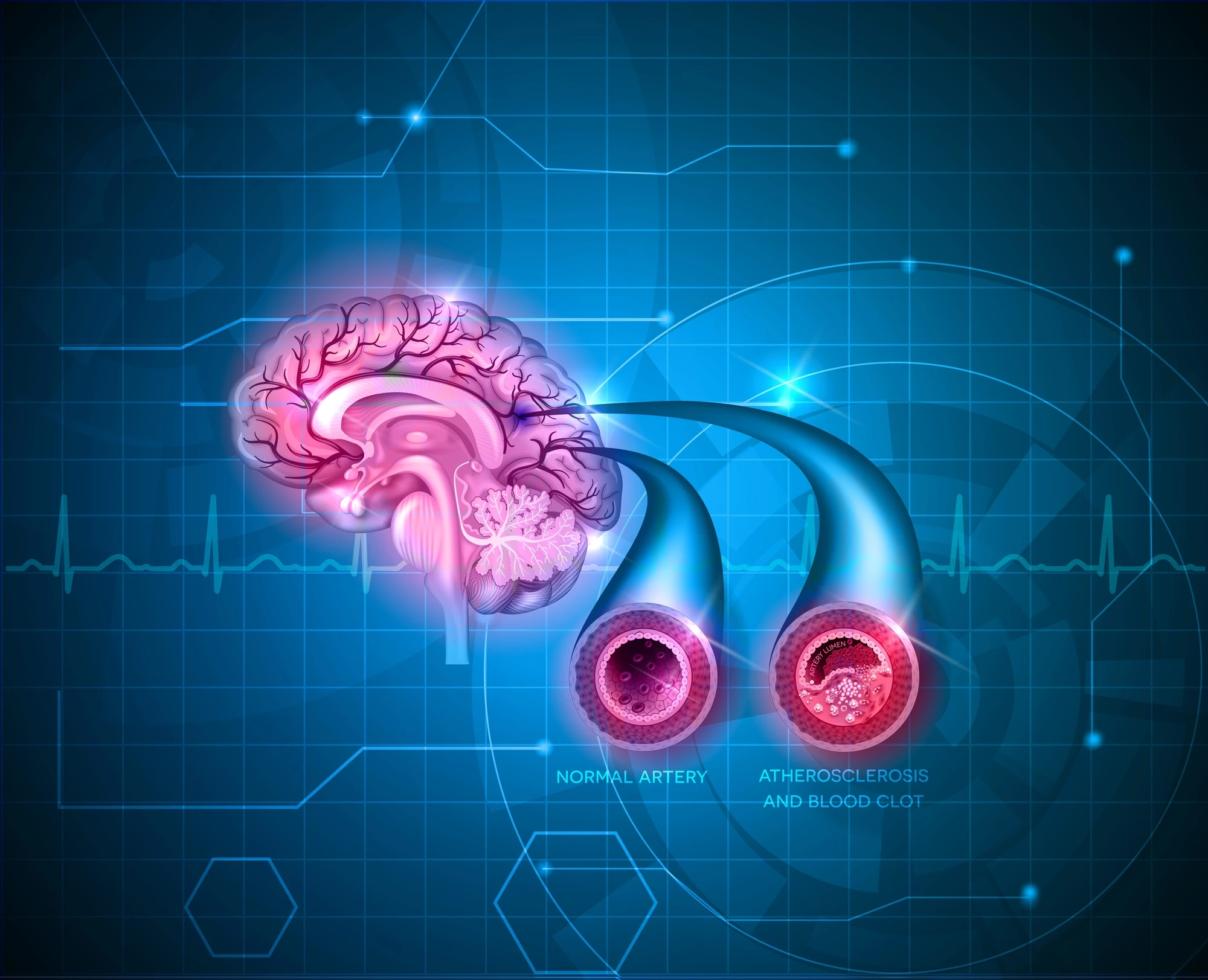
Patients suffering from a severe stroke are relatively easy to identify, however, the majority of strokes initially present with mild symptoms. Around one-third of strokes are initially missed by doctors, and the only way to conclusively detect the occurrence of a stroke is through resource-intensive MRI or CT scans.
“You would think that a stroke would be really obvious, and that’s true with severe strokes, but most strokes are actually minor (in terms of the initial symptoms),” explains Grant O’Connell, corresponding author on the new research. “Many people might just think that they’re having a bad migraine, so they don’t go to the hospital.”
O’Connell and his research team wanted to find out if a simple blood test could be developed to indicate whether a patient has suffered a minor stroke. Over recent years a number of studies have found specific proteins are released into the bloodstream following damage to brain tissue. In fact, the first blood test to detect the presence and severity of a traumatic brain injury (TBI) was approved by the U.S. Food and Drug Administration in 2018.
The Case Western researchers quickly discovered that despite there being a body of pre-existing knowledge linking certain proteins to brain damage, most of these biomarkers were not specific enough to a single condition to be used diagnostically.
“... what we’ve started to realize is that the proteins we study as candidate biomarkers had been identified some 20 to 40 years ago,” explains O’Connell. “And it turns out that a lot of these proteins aren’t as specific to the brain as we thought because we’re now seeing them expressed in other organs, so it could look like you’ve had a brain injury and you didn’t.”
So this new study set out to painstakingly algorithmically evaluate almost every protein-coding gene in the human genome to ascertain their potential for producing biomarkers relating to neurological damage. More than 17,000 protein-coding genes were studied, and a number of previously unexplored blood markers were revealed as potentially correlating with neurological damage.
To test the findings, blood was taken from a diverse group of patients suffering a variety of neurological conditions, including Alzheimer’s disease, ischemic stroke and multiple sclerosis. Alongside discovering some new biomarkers that correlate with general neurological damage, the research homed in on several proteins specifically linked to acute stroke.
One protein, called MT-3, was found to be especially promising in specifically identifying ischemic stroke. Elevated MT-3 levels were found to effectively discriminate between stroke patients and controls with an impressive 95 percent specificity and 70 percent sensitivity (specificity relating to negative rates and sensitivity measuring positive rates).
“If we had a blood test to tell us right away if someone is having a stroke, that could make a huge difference in patient care,” adds O’Connell.
This very early stage research is certainly promising, but a huge amount of work is needed before a stroke-detecting blood test appears in clinical use. O’Connell does point out the study’s findings could apply to more than just stroke, with the novel biomarker correlations detected in the genomic research pointing to possible new blood tests for large variety of neurological diseases, from multiple sclerosis to Alzheimer’s.
“This could open up the door to a whole new wave of biomarker research, and that could lead to clinically useful tests (if we can) validate the findings,” says O’Connell.
The new study was published in the journal PNAS.
Source: Case Western Reserve University