A human clinical trial examining the safety and efficacy of a "functional cure" for type 1 diabetes is currently underway. Trials of the novel islet cell replacement therapy developed by ViaCyte involve a device containing stem cells being implanted into a patient with type 1 diabetes. It's hoped these cells will then mature into human islet tissue with insulin-producing beta cells that produce insulin on demand.
So far, 2017 is proving to be an exciting year for breakthroughs in diabetes research, particularly in regards to treatments for type 1 diabetes. We have seen two very promising developments based in gene therapy, while a human trial for a type 1 diabetes vaccine is currently underway in Finland targeting a viral group known to trigger the disease.
The new treatment developed by ViaCyte is being described as a "functional cure" in that it could replace the missing insulin cells in a diabetic patient, as opposed to a more direct "cure" which would address the autoimmune roots of the disease.
The treatment being trialed piggybacks off prior working knowledge of islet cell transplantation being successful in patients with type 1 diabetes. For some time, patients with the disease have been treated with pancreatic cells from organ donors, successfully liberating them from insulin injections.
"Islet transplants have been used to successfully treat patients with unstable, high-risk type 1 diabetes, but the procedure has limitations, including a very limited supply of donor organs and challenges in obtaining reliable and consistent islet preparations," says trial investigator James Shapiro. "An effective stem cell-derived islet replacement therapy would solve these issues and has the potential to help a greater number of people."
The new treatment involves a device called PEC-Direct, which holds stem cell-derived pancreatic progenitor cells and is implanted into a patient. This allows those cells to mature in the body, becoming islet tissue that includes the beta cells that produce insulin when needed.
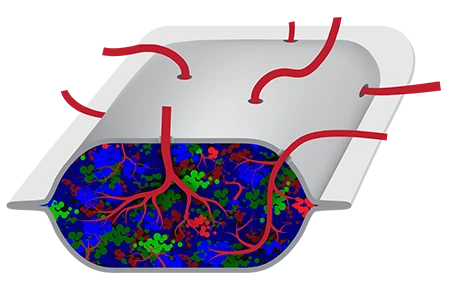
Because these stem cells can be replicated in a laboratory, this process doesn't rely on a finite amount of organ donor cells and allows the treatment to be delivered to a large number of patients quickly and easily. Unlike current similar treatments, which require invasive transplantation directly into the liver, this new device can be easily implanted superficially under the skin.
The first patients being implanted with small-format versions of the devices will evaluate the safety of the treatment. A second, larger cohort will be recruited later in 2017 to also evaluate its safety and also ascertain the treatment's efficacy. If implantation and cell maturation is demonstrated, the trials will measure how much clinically relevant insulin is being delivered by the treatment.
This new strategy being trailed by ViaCyte is hoped to have demonstrable and definite efficacy within the next two years, meaning the practical deployment may not be too far away if all goes well.
As well as the PEC-Direct for treating type 1 diabetes, the company is also developing a broader device called PEC-Encap, which could be used to treat all patients with diabetes who use insulin, type 1 and type 2. If these trials are successful they could prove to be a watershed moment in the treatment of diabetes.
Source: ViaCyte




