A massive study comparing the real-world effectiveness of three COVID-19 vaccines over eight months has detected protection from infection may decline but protection from death holds strong. Tracking nearly 800,000 US Veterans, the study found Johnson & Johnson’s single-dose vaccine showed the greatest decline.
“Our study gives researchers, policy makers and others a strong basis for comparing the long-term effectiveness of COVID vaccines, and a lens for making informed decisions around primary vaccination, booster shots, and other multiple layers of protection, including masking mandates, social distancing, testing and other public health interventions to reduce chance of spread,” explains Barbara Cohn, lead author on the study from the Public Health Institute.
The research looked at health records from around 780,000 veterans, spanning a period from February 2021 to October 2021. Vaccine effectiveness (VE) was measured by two metrics: protection from COVID-19 infection (VE-I) and protection from death (VE-D). The three COVID-19 vaccines approved for use in the United States were compared: Moderna, Pfizer and J&J.
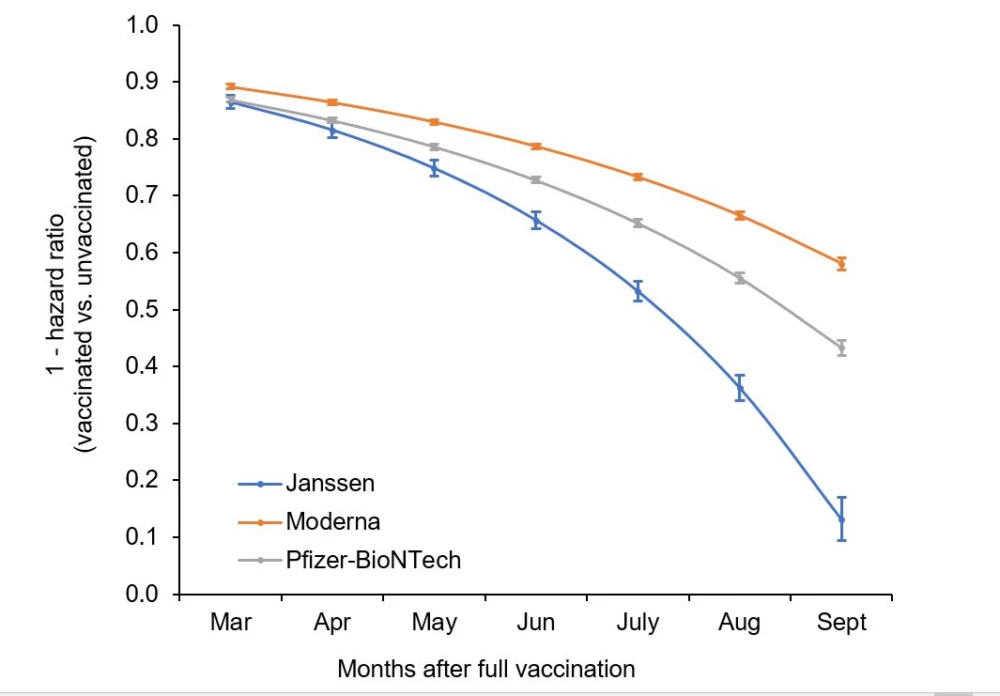
Overall, across the eight-month study period, vaccine protection against COVID-19 infection dropped from 87.9 percent to 48.1 percent. The biggest decline in VE-I was seen in the J&J vaccine, dropping from 86.4 percent to 13.1 percent. Pfizer’s protection against infection dropped from 86.9 percent to 43.3 percent, while Moderna performed best of the three going from 89.2 percent to 58 percent.
However, vaccine protection against death remained strong across the entire study period. With the spread of the Delta variant across the United States from July the study did not detect a significant decline in protection against death. Between July and October, vaccines were still 81.7 percent effective at preventing death from COVID-19 in those under the age of 65 and 71.6 percent effective in those over the age of 65.
Interestingly, for those under the age of 65 the Pfizer vaccine conferred the greatest protection against death (84.3 percent), with Moderna following at 81.5 percent and J&J at 73 percent. But in those over the age of 65 the Moderna vaccine was most effective at preventing death (75.5 percent), followed by Pfizer at 70.1 percent and J&J at 52.5 percent.
“Importantly, vaccination still provided protection against death in infected persons, and this benefit was observed for the Moderna, Pfizer-BioNTech, and Janssen (J&J) vaccines during the Delta surge, although the benefit was greater for Moderna and Pfizer-BioNTech compared to Janssen vaccines,” the researchers write in the newly published study. “Our findings support the conclusion that COVID-19 vaccines remain the most important tool to prevent infection and death.”
Another compelling finding in the study is the correlation between the rise of the Delta variant in the United States and the drop in vaccine protection against infection. Across all age groups the drop in protection from infection was profoundly steep from July. The researchers hypothesize this indicates the Delta variant may be responsible for this drop in VE-I instead of the vaccine itself becoming less protective over time.
This hypothesis echoes findings from another recent vaccine effectiveness study from the Centers for Disease Control and Prevention (CDC) and the New York State Department of Health. That research also detected declines in vaccine protection against infection during the weeks in July and August when the Delta variant rapidly spread across the country.
The CDC data indicated declines in VE-I plateaued across August and September once the Delta variant exceeded 85 percent prevalence. A statement from the New York State Department of Health speculated the increases in breakthrough infections over the past few months are most likely due to the Delta variant.
“These results suggest that declines in VE for infections occurred during the study time period but may have been driven primarily by factors other than immunological waning, such as the Delta variant or changes in COVID-19 prevention behaviors,” the statement notes.
Cohn says these findings affirm the importance of booster programs, especially in regards to the single-shot J&J vaccine. Cohn also argues the research points to the need for additional measures, beyond merely vaccination, in reducing the impact of COVID-19 over the coming months.
“… given the declines in vaccine protection and the dominance of the more infective Delta variant, we urge swift action to promote primary vaccination, boosters and to also encourage masking, social distancing and other layers of protection against infection,” says Cohn. “This is supported by our finding that breakthrough infections are not benign, but also by the strong evidence that vaccination still protects against death even for persons with breakthrough infections, compared to persons who become infected and are not vaccinated.”
The new study was published in the journal Science.
Source: PHI




