Researchers from The Mount Sinai Hospital have found changes to electrical activity in the heart can help predict which hospitalized COVID-19 patients are more likely to decline and die. The biomarker is easily measurable and potentially predicts death several days in advance.
When hospitals are overwhelmed with COVID-19 patients it can be challenging for doctors to work out where to best focus their limited attention and resources. A number of blood-based biomarkers have been found to help assess those patients most at risk of severe disease decline.
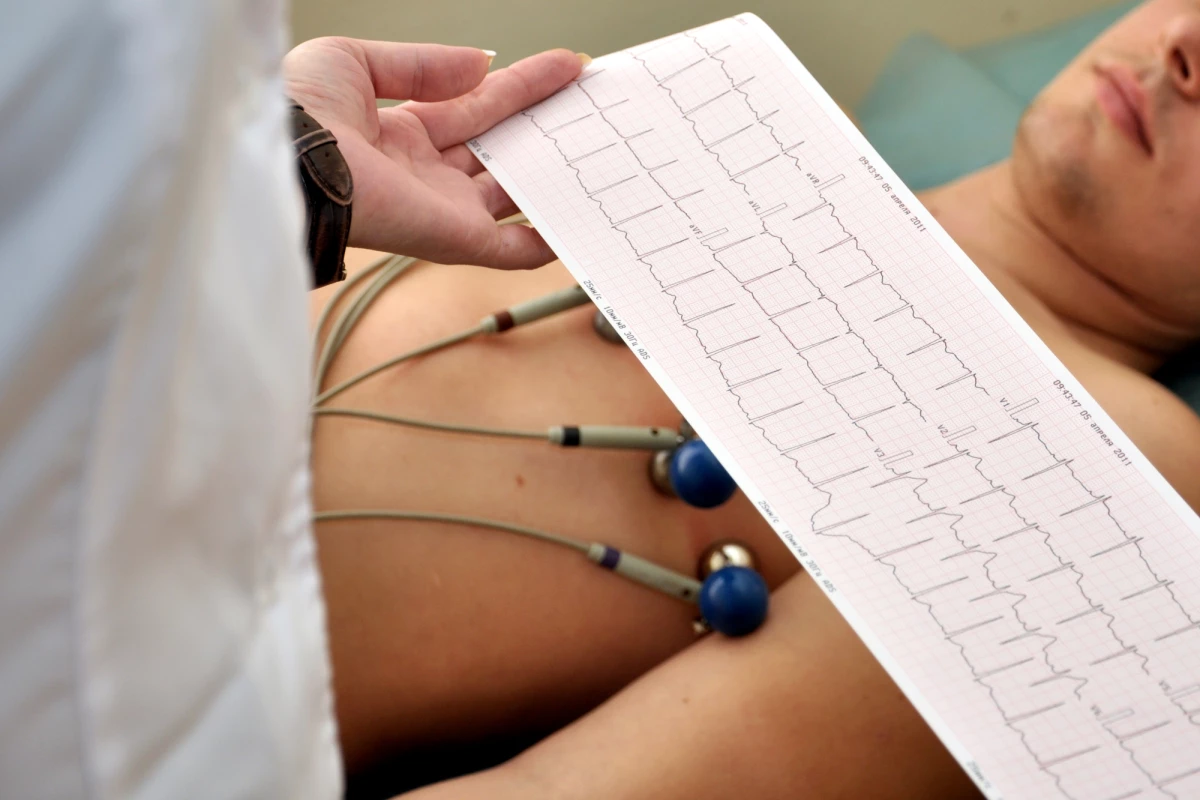
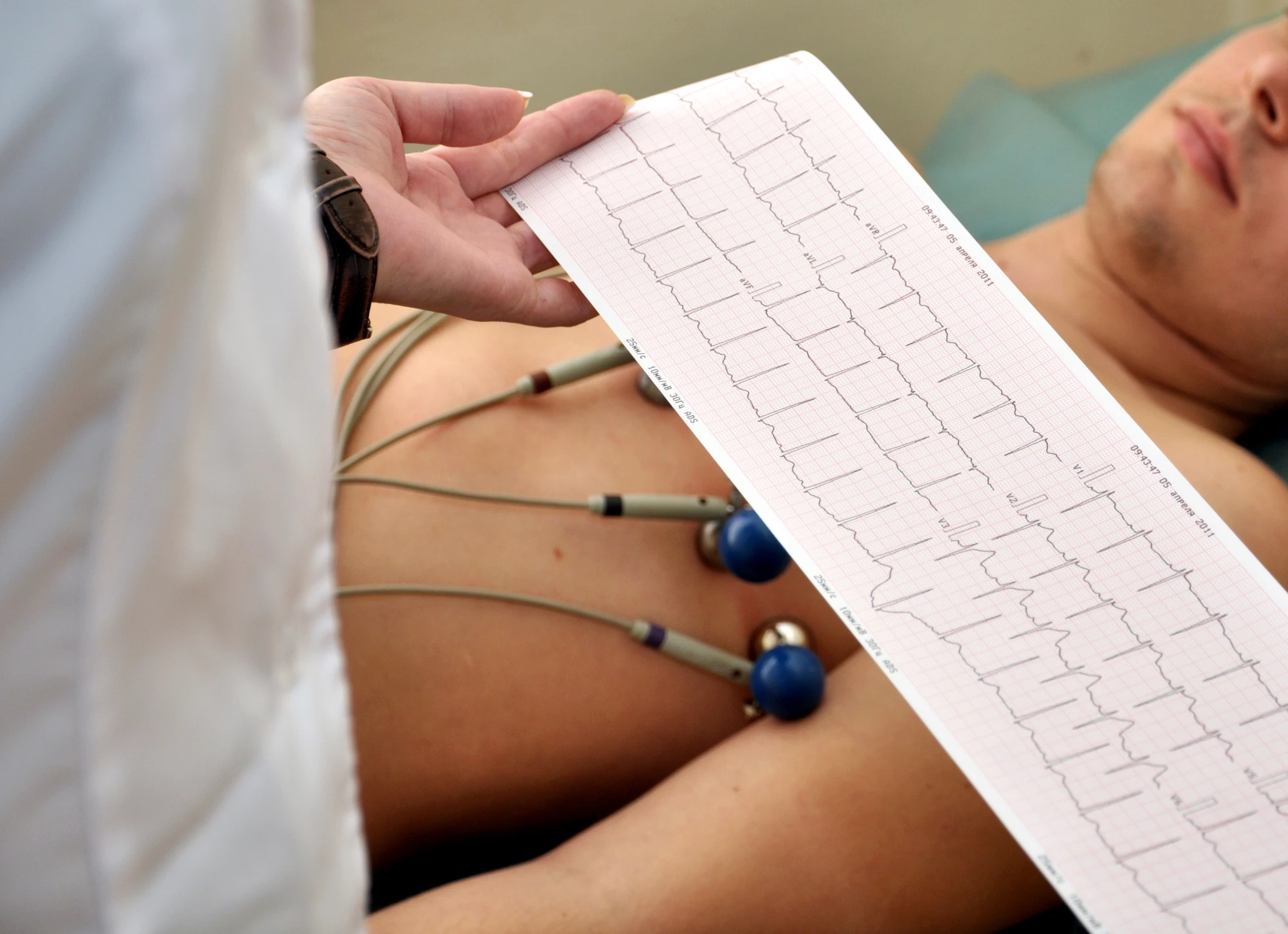
But blood tests take time to be collected and analyzed. This new biomarker can be measured using a simple electrocardiogram (EKG) machine, at a patient’s bedside. And the researchers claim it can predict whether a patient is likely to die at least two days in advance.
A retrospective investigation of health records from 140 COVID-19 patients revealed diminishing QRS waveforms were an indication of a patient declining in 74 percent of cases.
The criteria developed by the Mount Sinai team is dubbed LoQRS, and they propose it to be an effective way of triaging those patients most likely to decline. The median time to death from the first LoQRS reading detected in the study was 52 hours.
“Our study shows diminished waveforms on EKGs over the course of COVID-19 illness can be an important tool for health care workers caring for these patients, allowing them to catch rapid clinical changes over their hospital stay and intervene more quickly,” says Joshua Lampert, senior author on the new study. “With COVID-19 cases and hospitalizations continuing to rise again, EKGs may be helpful for hospitals to use when caring for these patients before their condition gets dramatically worse.”
Interestingly, the researchers also found LoQRS measures were effective in detecting those patients with influenza who were most likely to die. The median time to death from the first LoQRS measure in influenza patients, however, was around six days. The researchers point out this indicates COVID-19 is a much more virulent disease than influenza.
As LoQRS measures can only be detected over time across several EKG tests, Lambert proposes EKG measurements are taken for all COVID-19 patients when they are initially admitted.
“When it comes to caring for COVID-19 patients, our findings suggest it may be beneficial not only for health care providers to check an EKG when the patient first arrives at the hospital, but also follow-up EKGs during their hospital stay to assess for LoQRS, particularly if the patient has not made profound clinical progress,” says Lampert. “If LoQRS is present, the team may want to consider escalating medical therapy or transferring the patient to a highly monitored setting such as an intensive care unit (ICU) in anticipation of declining health.”
The new study was published in the American Journal of Cardiology.
Source: Mount Sinai