The human body is good at replenishing cells to repair damage, but one vital organ lacks this ability – the heart. But now, researchers at the University of Texas Southwestern Medical Center have uncovered a suite of proteins in mice that could be switched off to induce heart cells to begin replicating again temporarily.
Part of what makes heart disease so deadly is that even if a person survives the initial heart attack, the organ’s function is permanently impaired. Damaged cells can’t be replaced so instead scar tissue forms, which doesn’t beat and eventually leads to further attacks.
But that may not always be the case. Previous studies by the team found that, in mice at least, the heart can regenerate for the first few days after birth, but the function grinds to a halt after about a week. The researchers wanted to find out why that was, and whether it could be undone.
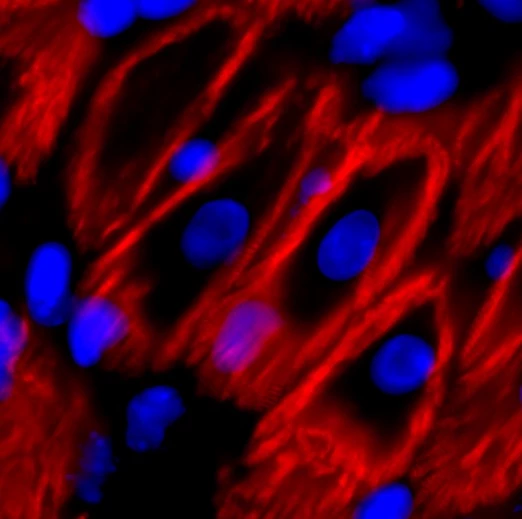
For the new study, the team identified a set of proteins that appear to stop heart cell division – and found that switching them off can restart the division process temporarily. The proteins in question are transcription factors called Meis1 and Hoxb13, and another protein called calcineurin.
The team originally thought that Meis1 acted alone, and in earlier work they deleted the gene that encodes this protein in mice. That did extend how long the hearts of the young mice could replenish cells, but not for too much longer.
The researchers later found a related protein, Hoxb13, that acts as a kind of chaperone for Meis1. When this was deleted, the young mice had a similar extended period of heart cell division, but not long enough to be much use.
Next, the team tested switching off Hoxb13 in adult mice after inducing heart attacks. Heart cells began dividing again for a short time but, while it prevented deterioration, it wasn’t enough to help the mice fully recover.
Interestingly, switching off both Meis1 and Hoxb13 worked better. In this case, the team noted that heart cells shrank and began multiplying at a faster rate, mimicking an earlier stage of development. That helped the animals regain almost normal heart function after an induced heart attack.
While this study is of course only applicable to mice at the moment, the long-term hope is that scientists may be able to develop drugs that can be given to a patient after a heart attack to help heal the organ and prevent further damage. Even just a temporary boost in the ability for heart cells to divide could drastically improve patient outcomes.
The best bet for this may come from a third protein, calcineurin, which the team found to regulate Meis1 and Hoxb13. Drugs already exist to target this protein, since it plays a role in many other diseases, so it could be adapted for heart attack patients.
“By building up the story of the fundamental mechanisms of heart cell division and what blocks it, we are now significantly closer to being able to harness these pathways to save lives,” says Hesham Sadek, lead researcher on the study.
Other experimental methods to get heart cells replenishing themselves again involve using placental stem cells, applying nanofiber patches, reprogramming structural cells to become heart muscle cells, or ramping up expression of certain genes.
The new research was published in the journal Nature.
Source: UT Southwestern




