Stem cell transplants are often used to treat blood cancers, but the process can be risky. In a new study in mice, researchers at Washington University in St. Louis have developed a way to make the process safer by targeting a patient’s faulty stem cells more precisely, removing the need for radiation or chemotherapy.
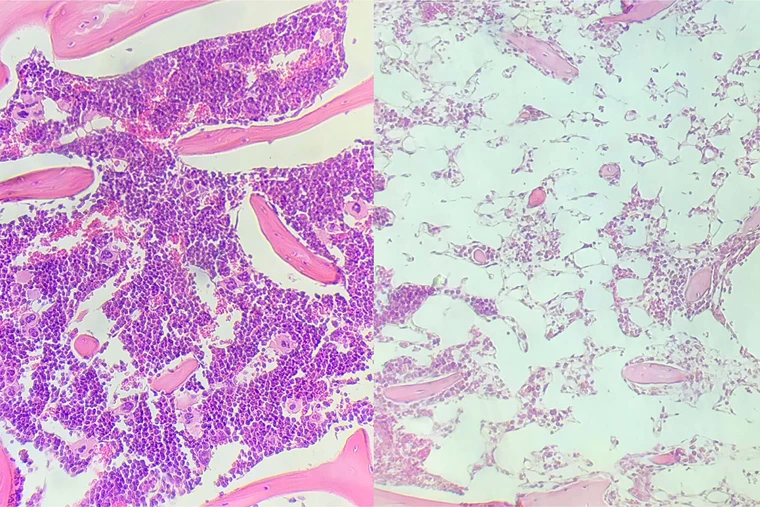
Leukemia and other blood cancers typically start in the bone marrow, where blood cells are produced by stem cells. For those with life-threatening illness, there’s one treatment option that can be very effective, but carries a serious risk of side effects – hematopoietic stem-cell transplantation (HSCT).
To prepare their body for donated stem cells, a patient is first given radiation or chemotherapy, which kills their own stem cells, destroys remaining cancer cells, and weakens their immune system to prevent rejection. That boosts the chances that the new stem cells will take hold, and the procedure can functionally cure some patients of the disease. But it also puts them at high risk of infection or a dangerous condition called graft-versus-host disease, where immune cells from the implanted tissue attack the patient’s own cells.
In the new study, the researchers developed a technique that doesn’t require radiation or chemotherapy. Instead, the stem cells in bone marrow are targeted for destruction more precisely, using molecules called antibody-drug conjugates (ADCs). These bind to specific proteins on the surface of blood stem cells, which the team says keeps them from harming other cells. Once they reach their target, the ADCs release a drug called saporin to kill the stem cells.
After the donor stem cells are transplanted, immunosuppressive drugs are still required to prevent rejection. In this case the team used a drug called baricitinib, which is currently used to treat rheumatoid arthritis.
In tests in mouse models of leukemia, the technique resulted in successful stem cell transplants. The combination of ADCs with baricitinib prevented the test animals’ immune cells from attacking the new stem cells, and they didn’t develop graft-versus-host disease because the immunosuppressants prevented it. Treated mice also maintained normal blood cell counts throughout treatment, sidestepping another common side effect of existing transplantation methods. The key difference, the team says, is that radiation or chemotherapy kills all of the stem cells at once, while the new technique replaces them more slowly.
Importantly, the slower treatment meant that the immunosuppressants could be reduced over time, and were not needed at all after the donor stem cells had completely replaced the patient’s own.
The team says that with more work in animal studies and eventually human trials, the treatment could one day be applied to patients with leukemia and other blood cancers, as well as other diseases for which the current method is considered too extreme a response.
“To be able to do a stem cell transplant without having to give radiation or chemotherapy would be transformative,” says John DiPersio, senior author of the study. “It could eliminate the dangerously low blood cell counts, bleeding complications, organ damage, and infections. It has particular implications for conducting bone marrow transplantation or gene therapy for patients with noncancerous diseases such as sickle cell anemia, where the toxicities of chemotherapy- or radiation-associated conditioning are important to avoid. We have more work to do before we’re ready to translate these findings to people, but we’re encouraged by the results of this study.”
The research was published in the Journal of Clinical Investigation.




