Scientists have discovered how a unique kind of cell death, due to iron toxicity, creates a snowball effect that advances cognitive decline. With this finding, a whole new approach to treatment could be developed.
In the study, Oregon Health & Science University (OHSU) researchers have for the first time identified how ferroptosis, a type of cell death caused by a buildup of iron, destroys the brain’s immune cells in Alzheimer’s disease and vascular dementia.
“This is a major finding,” said senior author Dr Stephen Back, neuroscientist and professor of pediatrics in the OHSU School of Medicine.
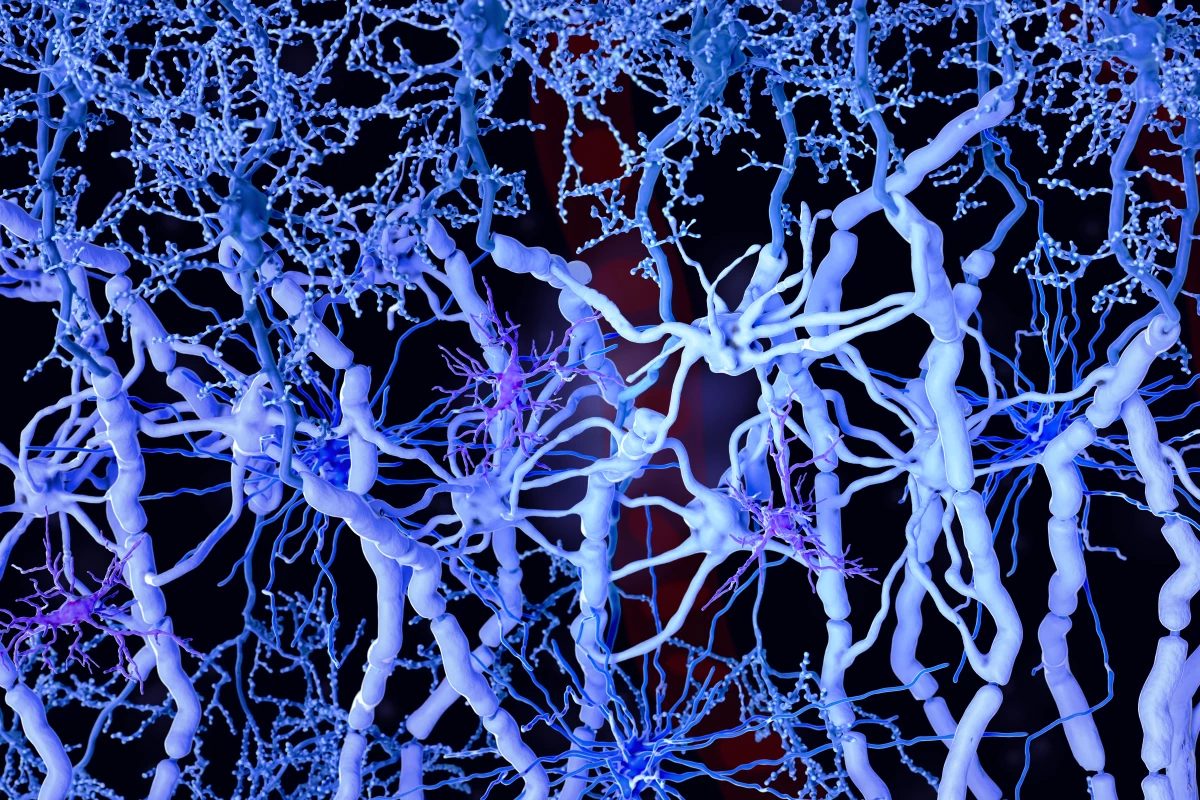
Looking at post-mortem brain tissue from dementia patients, the team found that these immune cells, microglia, were being killed while trying to go about their routine business of cleaning out debris. However, in this case, the debris is made from pieces of iron-rich myelin, which forms the protective layer around nerves that can get damaged and break down during neurological distress. This triggers ferroptosis, or the death of the first-responder microglia cells, in the brain’s white matter.
“Everyone knows that microglia are activated to mediate inflammation,” Dr Back said. “But no-one knew that they were dying in such large numbers. It’s just amazing that we missed this until now.”
While suppressing ferroptosis has been tabled as a target for Alzheimer’s before, these new insights have huge potential for new therapeutics to slow the progression of neurodegenerative diseases.
“We’ve missed a major form of cell death in Alzheimer’s disease and vascular dementia,” Dr Back said. “We hadn’t been giving much attention to microglia as vulnerable cells, and white matter injury in the brain has received relatively little attention.”
The researchers believe their findings should point drug companies in the direction of developing compounds that limit microglial degeneration.
“That’s where the field will go next,” he said. “A discovery like ours will stimulate a lot of excitement in the pharmaceutical industry to develop therapeutically important compounds.”
They also note that intervention is key; cognitive decline is a slow road that usually begins after a period of low blood flow and oxygen to the brain due to stroke or chronic conditions like hypertension and diabetes.
“Dementia is a process that goes on for years and years,” Dr Back said. “We have to tackle this from the early days to have an impact so that it doesn’t spin out of control.”
The study was published in the journal Annals of Neurology.