Viruses firmly hold the world’s attention at the moment, but we shouldn’t ignore the rising health threat that bacteria pose, too. The crafty critters are fast evolving resistance to antibiotics, meaning our best drugs could soon stop working entirely. Now researchers in Australia have found a way to bypass drug resistance in these so-called superbugs – by distracting them with predatory viruses.
Antibiotics were one of the most important medical breakthroughs of the 20th century, saving countless lives by clearing out infections that previously may have been lethal. Unfortunately, we’ve been locked in a biological arms race ever since, as bacteria develop better and better defenses against the drugs.
And the tide is slowly turning in their favor. Our last line of defense is already beginning to fail, with some bacteria now impervious to anything we can throw at them. Studies have predicted that if this trend continues, superbugs could kill as many as 10 million people a year by 2050.
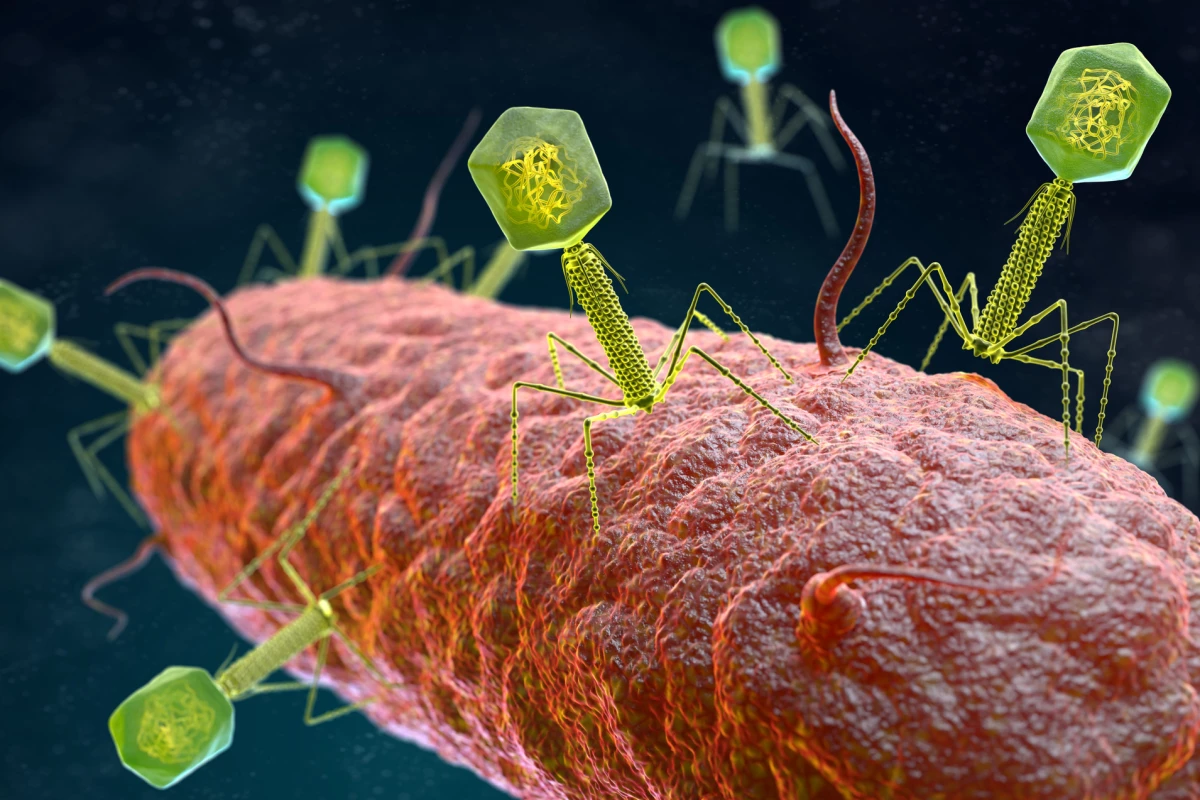
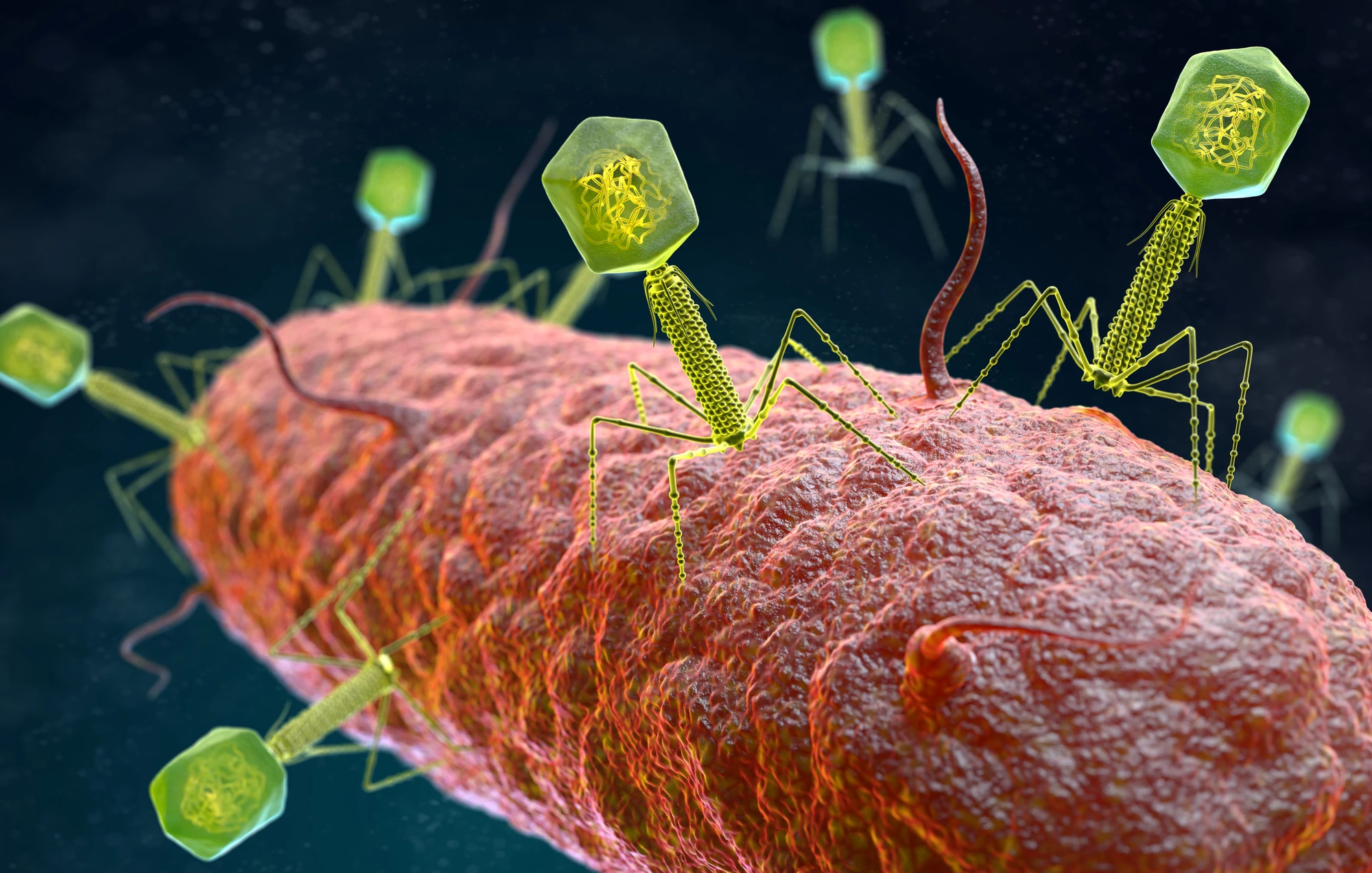
In an effort to find new treatments, scientists are beginning to circle back to old, discarded ideas. At the top of the list is phage therapy, which uses bacteriophages – tiny viruses that prey solely on bacteria – to hunt down the superbugs. Since antibiotics were discovered soon after phages were, there was never a dire need to develop phage therapy further. Until now.
For the new study, researchers from Monash University set out to find a phage that would target and kill a superbug called Acinetobacter baumannii. This opportunistic bacteria, often acquired in hospitals, is currently priority target number one on the World Health Organization’s hit list.
The team identified a phage from wastewater that almost completely wiped out A. baumannii in lab culture tests. Unfortunately, the effect was short-lived, and it only took a few hours before the bacteria developed resistance to the phages. But there’s an intriguing upside to the story: in developing resistance to phages, the bacteria became vulnerable to antibiotics again.
"A. baumannii produces a capsule, a viscous and sticky outer layer that protects it and stops the entry of antibiotics," says Gordillo Altamirano, lead author of the study. "Our phages use that same capsule as their port of entry to infect the bacterial cell. In an effort to escape from the phages, A. baumannii stops producing its capsule; and that's when we can hit it with the antibiotics it used to resist."
In tests, the phage therapy was found to resensitize the bacteria to at least seven different antibiotics that it was once resistant to. Phage therapy proved effective in tests on mice, raising hopes that the two could work well as a team in the future.
The research was published in the journal Nature Microbiology.
Source: Monash University