New research presented at the American Society for Pharmacology and Experimental Therapeutics annual meeting has demonstrated the potential for genetically engineered bacteria to be an effective Parkinson’s disease treatment. The researchers created a bacteria that can synthesize a consistent source of medicine inside a patient’s gut, and animal tests have demonstrated it is safe and effective.
The idea of engineering bacteria to serve as medical treatments is not new. For years scientists have experimented with ways of modifying bacteria to fit our needs, from engineering bacteria to eat up excess ammonia in a human body to helping bacteria hunt down colorectal cancer cells.
Of course, before an idea like this is ready for mainstream clinical uses a number of hurdles need to be overcome. It's one thing to offer a patient controlled doses of a drug via a pill, but limiting the growth of living microbes engineered to synthesize those same therapeutic molecules in the human gut is a whole different challenge.
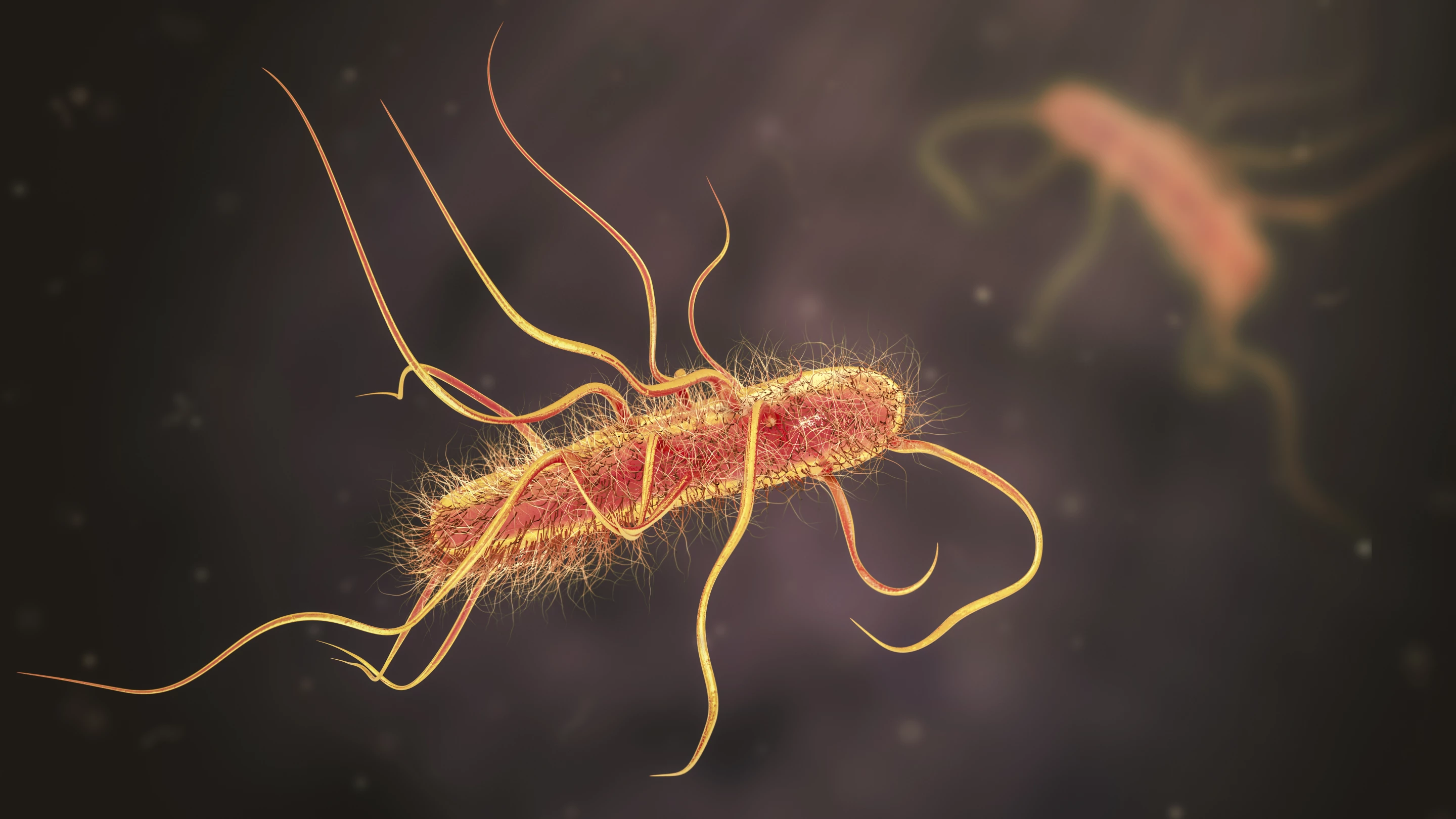
New research from a team of scientists has presented an incremental step forward in engineering a novel strain of the human probiotic E.coli Nissle 1917 that has been developed to continually synthesize a Parkinson’s disease drug known as L-DOPA.
L-DOPA is a molecule that acts as a precursor to dopamine and it has been the gold-standard treatment for Parkinson’s patients for decades. Doctors have found that after around five years of L-DOPA treatment patients often develop side effects known as dyskinesias. These side effects are thought to be related to the lack of a continuous source of the drug to the brain.
So to address this problem the new research explored whether bacteria producing L-DOPA in the gut could result in a consistent delivery of the drug to the brain. Piyush Padhi, a researcher working on the project, said the engineered bacteria eat up a molecule called tyrosine and spit out L-DOPA.
"After several iterations and improving gut microbiome-based drug delivery technology, we have developed a gut-healthy probiotic bacteria that can produce stable levels of L-DOPA in a way that can be highly tuned to deliver the dose required for each patient," Padhi explained.
Several mouse studies demonstrated that the engineered bacteria resulted in steady, consistent blood concentrations of L-DOPA. Then experiments with Parkinson’s disease animal models found the treatment led to improved motor and cognitive functions, indicating the engineered bacteria were producing therapeutically effective volumes of the drug.
The researchers also claim the levels of L-DOPA produced by the bacteria can be finely controlled. This can be done by either limiting the daily doses of bacteria consumed in capsules or by modulating consumption of a sugar called rhamhose. This rare sugar is needed by the bacteria to go on and produce L-DOPA.
Anumantha Kanthasamy, another researcher working on the project, said the team is working on adapting the approach to treat other diseases that require continual measured doses of drugs. The next step is optimizing the engineered bacteria as the research looks to human trials.
"We are hoping that our continuous, non-pulsatile microbial-based delivery method for L-DOPA limits the development and progression of levodopa-induced dyskinesia," said Kanthasamy. "We are currently exploring using this approach to deliver treatments for other conditions such as Alzheimer's disease and depression and are in process of initiating FDA approval for clinical testing of this novel gut microbiome therapeutic technology."
The new research has yet to be published in a peer-reviewed journal but was recently presented at the American Society for Pharmacology and Experimental Therapeutics annual meeting during the Experimental Biology (EB) 2022 meeting in Philadelphia.
Source: Experimental Biology