As common as the common cold is, it’s been notoriously difficult to actually cure. That’s largely because there are so many different viruses in the same family, and they can mutate quickly to get around our best efforts. Now, a new study shows that disabling a single protein in human cells could render the cold virus ineffective.
Viruses, like those that cause colds and flu, are some of the fastest-evolving forms of life on Earth. That’s why there are no permanent cures for these common illnesses. Any time scientists come up with a vaccine, it doesn’t affect all strains of the virus and even those that are inhibited by it can evolve resistance to the drug pretty quickly.
While many researchers are experimenting with the biology of the viruses themselves to find new weaknesses, a new study by scientists at Stanford and the University of California San Francisco (UCSF) may have found a target on the cells they infect instead.
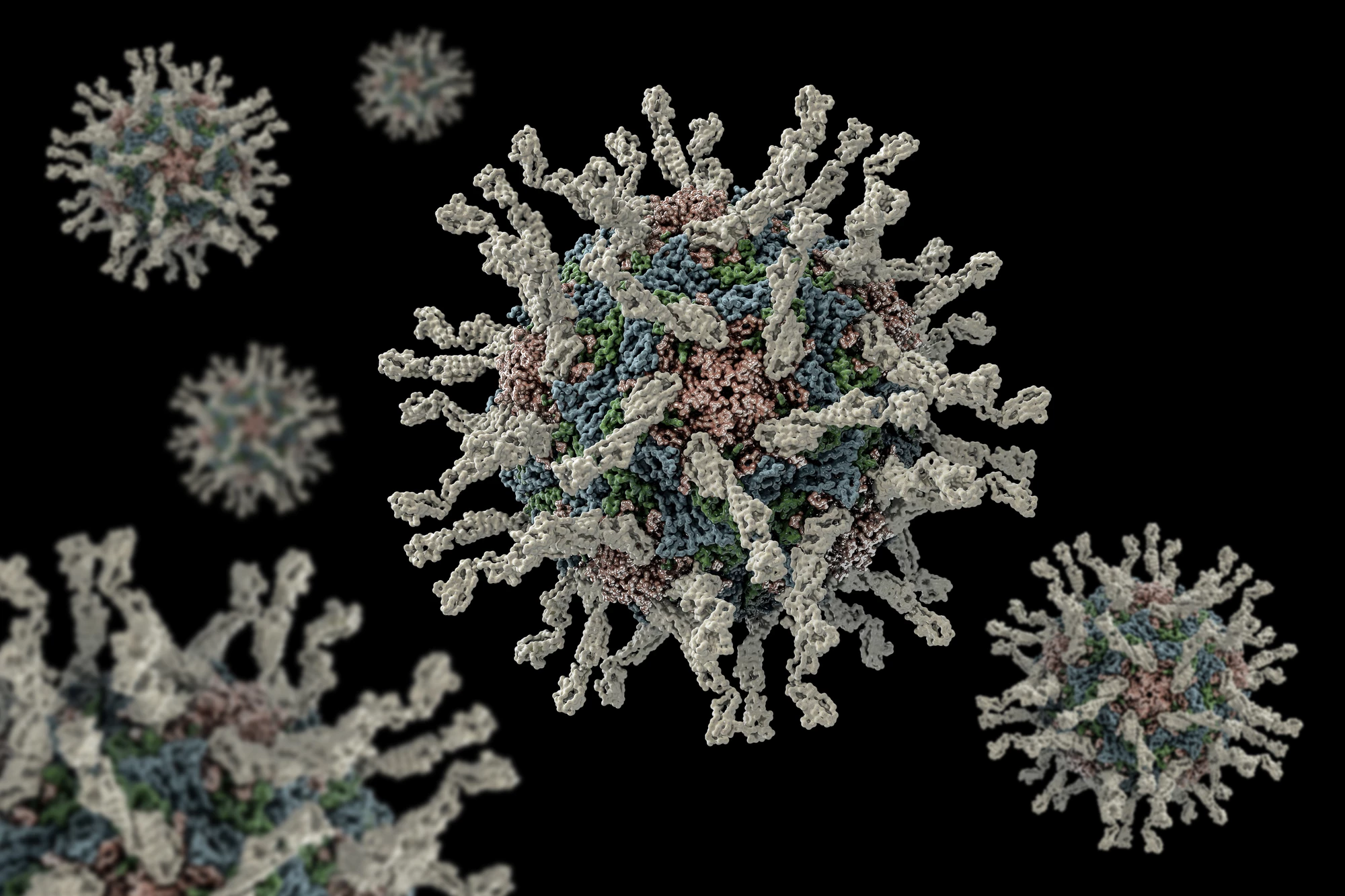
Many of the viruses that cause colds belong to the rhinovirus family, which in turn are types of enteroviruses. These viruses infect human cells by taking advantage of different proteins in the cell. So the researchers investigated which of those proteins the viruses were using, and set out to block those.
The team started by growing cultures of human cells, with each culture gene-edited to knock out a single gene that codes for a protein that viruses might use. Then they introduced two different viruses – RV-C15, which can trigger people’s pre-existing asthma, and EV-D68, which is linked to a severe, polio-like disease called acute flaccid myelitis.
By systematically switching off different genes, the researchers could see which proteins the viruses were relying on to infect the cells. They found many genes that, when turned off, could inhibit infection by one virus, but only very few managed to put a stop to both at once.
One particularly promising gene encoded for an enzyme called SETD3. The team grew a culture of human cells that lacked SETD3 and then tried to infect them with many different enteroviruses, including EV-D68, poliovirus, three types of rhinoviruses and two types of coxsackievirus. None of these viruses could replicate without SETD3, which worked out to about 1,000 times better protection than control cells.
In further tests on human bronchial epithelial cells – those in the nose and airways, where colds take hold – the replication was cut 100-fold.
As promising as these results may be, not much is known about SETD3. Its role in the body is largely unknown, so simply cutting it out may have unintended health consequences. To investigate, the researchers engineered mice that completely lacked the enzyme. These mice grew up to be healthy adults that could still reproduce, but had the added bonus of being able to resist infection by dangerous enteroviruses. The team even injected the viruses directly into the mouse brains soon after birth, but the animals were unaffected.
“In contrast to normal mice, the SETD3-deficient mice were completely unaffected by the virus,” says Jan Carette, senior author of the study. “It was the virus that was dead in the water, not the mouse.”
Of course, we’re not mice, so there’s no guarantee that these results will end up being safe or effective in humans. While it’s far from a catch-all cure for the common cold, the research is an interesting new avenue that might someday lead to new breakthroughs.
The research was published in the journal Nature Microbiology.
Source: Stanford